What treatment options are available?
Nonsurgical Rehabilitation
Physical therapy at STAR Physical Therapy can be very useful for patients with SI joint pain. Your physical therapist will assess your SI joint dysfunction and determine how much of your pain is coming directly from this joint. They will then determine how well the joint is moving. The joint can be moving well, or there can be too much movement (hypermobile) or not enough movement (hypomobile.) Your individual physical therapy treatment will be determined according to these findings.
Regardless of whether your SI joint pain is determined to come from a hyper or a hypomobility, your therapist may use heat, ice, or electrical modalities such as ultrasound or interferential current to help decrease your pain initially. They may also massage around the back, buttocks, and hip areas to also provide relief by relaxing tight muscles that could be pulling in the area of the SI joint. In addition, your physical therapist will ask you to limit or modify those activities, if possible, that irritate your SI pain. A short period of resting from these activities can help to calm the an irritated joint.
When movement of a joint is limited, encouraging more motion can ease the pain. If you don't have full range of motion, your therapist has several methods to help you assist in increasing the movement at your SI joint. These methods may include using joint mobilizations or manipulations, performing passive stretching, and massaging any tight muscles. Stretches and strengthening exercises as part of a home program will also be given as they can assist to help mobilize your own stiff SI joint. These exercises may be targeted at your SI joint directly, but will also include exercises for your low back, abdominals and core area, buttocks and hips, groin, and the front and back of your thighs. These areas immediately around the SI joint are crucial in supporting the pelvis and the joint itself. Having a stiff low back or stiff hip in particular can significantly increase the stress put through your SI joints, so improving the mobility in these areas will certainly be focused on. Maintaining a strong core muscular area is also particularly important in easing the discomfort that comes from SI joint pain, so exercises for this area will also be focused on.
If your SI joint is deemed to have too much relative mobility our physical therapy treatment is aimed at helping to stabilize the SI joint. Specific strengthening exercises will be taught in order to improve strength in muscles that support the SI joint such as certain muscles of the low back, the abdominal and core area, the groin, and the deep and superficial buttocks muscles. Developing muscular endurance in these areas is just as important as developing strength. The SI joint is put under stress during nearly every activity that you undertake, even sitting or rolling in bed, so the ability to support the joint’s alignment for long periods of time is crucial. Any deviation from correct biomechanics even for short periods can potentially put stress on the SI joint and cause discomfort, particularly if the joint is already irritable. Specific stretching exercises will also be prescribed in order to ease off the pull of tight muscles around the joint.
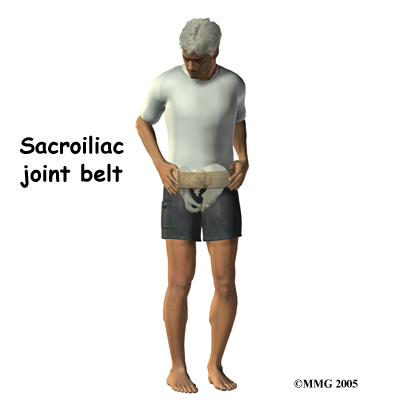
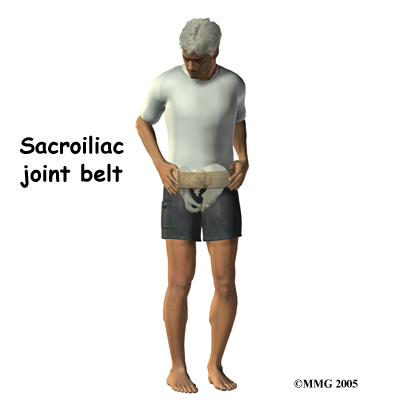
Unfortunately, few muscles actually connect to both the sacrum and the pelvis and therefore although you strengthen the weak muscles, stabilizing the SI joint completely can be more difficult in comparison to stabilizing other joints. Your SI joint may continue to move relatively more than normal and cause you ongoing discomfort with certain activities or when your muscles get tired. To combat this overall increased motion and to aid in alignment your therapist may suggest that you use a SI belt to help stabilize the joint. An SI belt is worn over the SI joints and around the hip area to help compress the joint together in order to create increased stability. Wearing an SI belt can often ease pain during activity and allow you to exercise comfortably. Many pregnant women find these belts particularly helpful. Using tape on the SI joint area, hips, and low back can also help to ease some of your pain, so your therapist may try doing this either before suggesting a belt, or in conjunction with doing so.
As with any injury or biomechanical dysfunction, maintaining one’s posture and alignment is very important. Despite whether your therapist determines that your SI joint has increased or decreased motion, they will be strict in encouraging you to maintain proper posturing and alignment at all times. Maintaining good posture can significantly decrease the stress put through the SI joints. By improving the endurance of the muscles that support the SI joint, you will be able to maintain your posture and alignment for longer periods of time, and lengthen the time frame between painful bouts of SI joint irritation.
Other Nonsurgical Treatments
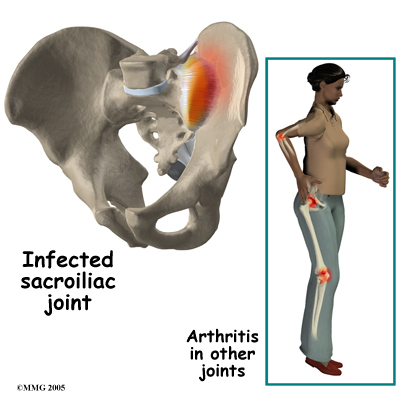
Anti-inflammatory medications, such as ibuprofen and naproxen, are commonly used to treat the pain and inflammation in the SI joint. Acetaminophen or paracetamol can be used to treat the pain, but it will not control the inflammation.
If conservative treatment is unsuccessful, your doctor may suggest injections to the joint. As described above, injections are used primarily to confirm that the pain is coming from the SI joint but they can also be useful in controlling the pain. A series of cortisone injections may be recommended to try to reduce the inflammation in and around the SI joint. Cortisone is a powerful anti-inflammatory medication that is commonly used to control pain from arthritis and inflammation. Other medications have been injected into the joint as well. A chemical called hyaluronic acid has been used for years to treat osteoarthritis of the knee. This chemical is thought to reduce pain due to its lubricating qualities and its ability to nourish the articular cartilage in the synovial joints. The true mechanism of action remains unknown, but it has been used with some success in the SI joint. All of these injections, unfortunately, are temporary and are expected to last several months at the most.
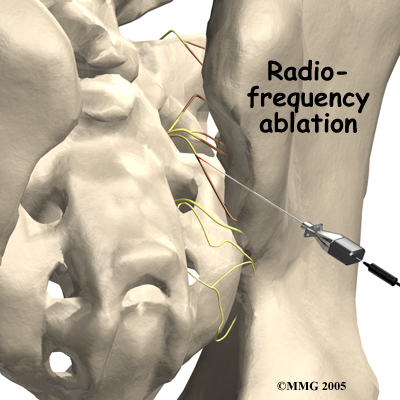
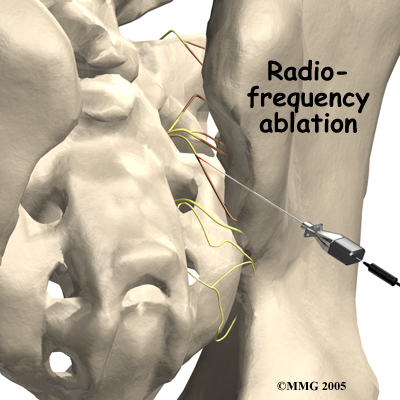
Another procedure that has been somewhat successful for chronic SI joint pain is called radiofrequency ablation. After a diagnostic injection has confirmed that the pain is coming from the SI joint, the small nerves that provide sensation to the joint can be "burned" with a special needle called a radiofrequency probe. In theory, this destroys any sensation coming from the joint, making the joint essentially numb. Unfortunately this procedure is not always successful. If it does help, it is temporary but can last for up to two years and can be repeated if needed.
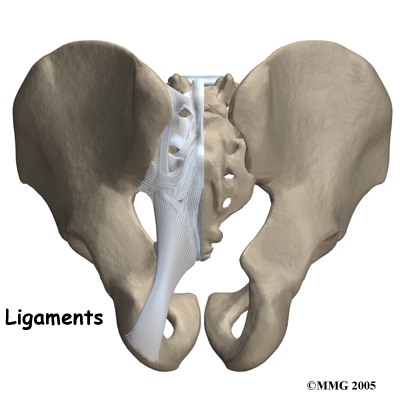
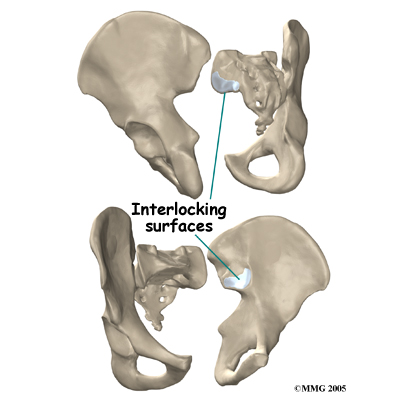 The SI joint is one of the larger joints in the body. The surface of the joint is wavy and fits together similar to the way Lego® pieces fit together. Very little motion occurs in the SI joint compared to most other joints. The motion that does occur is a combination of sliding, tilting and rotation. The most that the joint moves in sliding is probably only a couple of millimeters, and may tilt and rotate two or three degrees.
The SI joint is one of the larger joints in the body. The surface of the joint is wavy and fits together similar to the way Lego® pieces fit together. Very little motion occurs in the SI joint compared to most other joints. The motion that does occur is a combination of sliding, tilting and rotation. The most that the joint moves in sliding is probably only a couple of millimeters, and may tilt and rotate two or three degrees.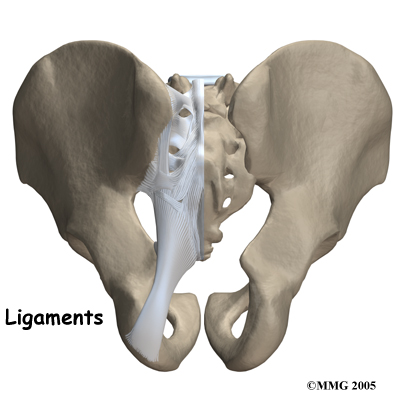
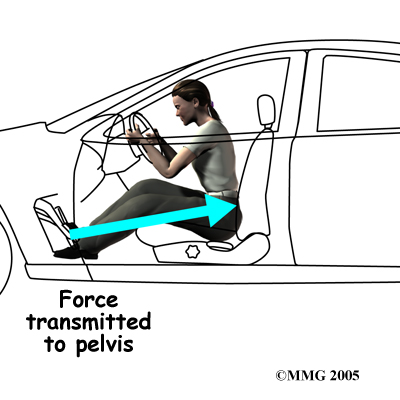
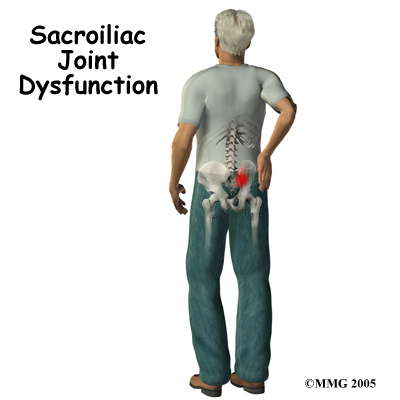
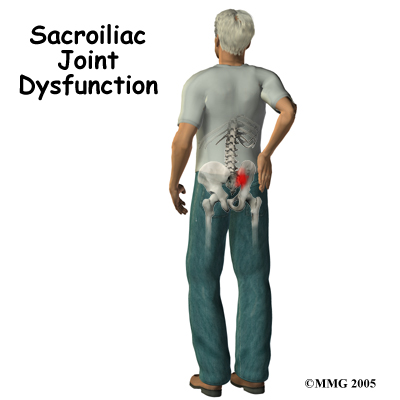 Most commonly the pain from an SI joint dysfunction is either directly over the SI joint itself or may radiate pain lower down into the buttocks. The pain may affect one side or both SI joints. Most times the pain from an irritable SI joint remains well above the knee, but in a few cases it can radiate down the leg all the way to the foot and may be confused with a herniated disc of the lumbar spine. The pain may also radiate into the groin area. People often feel muscle spasm or tightness in one or both of their buttocks muscles when the SI joint is affected.
Most commonly the pain from an SI joint dysfunction is either directly over the SI joint itself or may radiate pain lower down into the buttocks. The pain may affect one side or both SI joints. Most times the pain from an irritable SI joint remains well above the knee, but in a few cases it can radiate down the leg all the way to the foot and may be confused with a herniated disc of the lumbar spine. The pain may also radiate into the groin area. People often feel muscle spasm or tightness in one or both of their buttocks muscles when the SI joint is affected.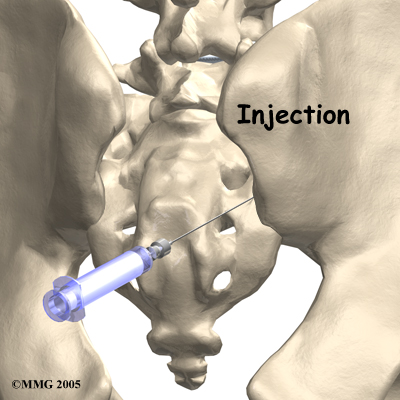
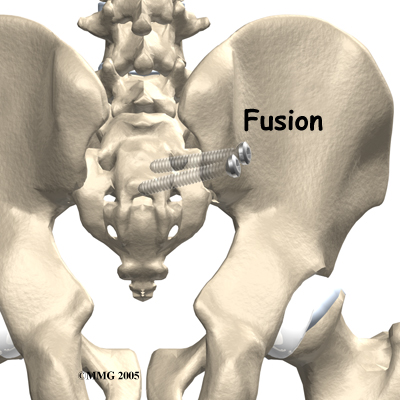
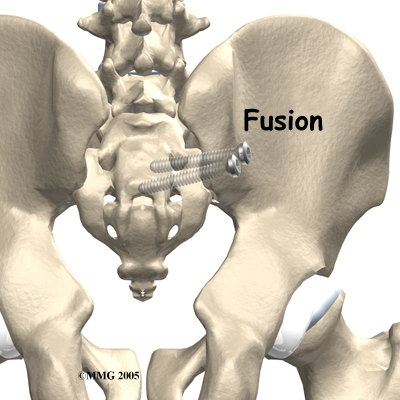 You will normally need to wait at least six weeks before beginning rehabilitation at STAR Physical Therapy after having SI joint fusion surgery. You should plan on attending therapy sessions for six to eight weeks but you can expect full recovery to take up to six months.
You will normally need to wait at least six weeks before beginning rehabilitation at STAR Physical Therapy after having SI joint fusion surgery. You should plan on attending therapy sessions for six to eight weeks but you can expect full recovery to take up to six months.