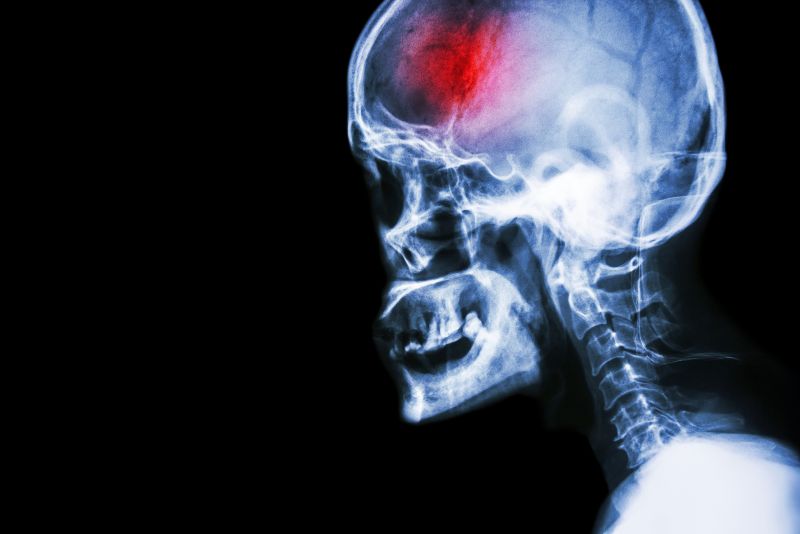
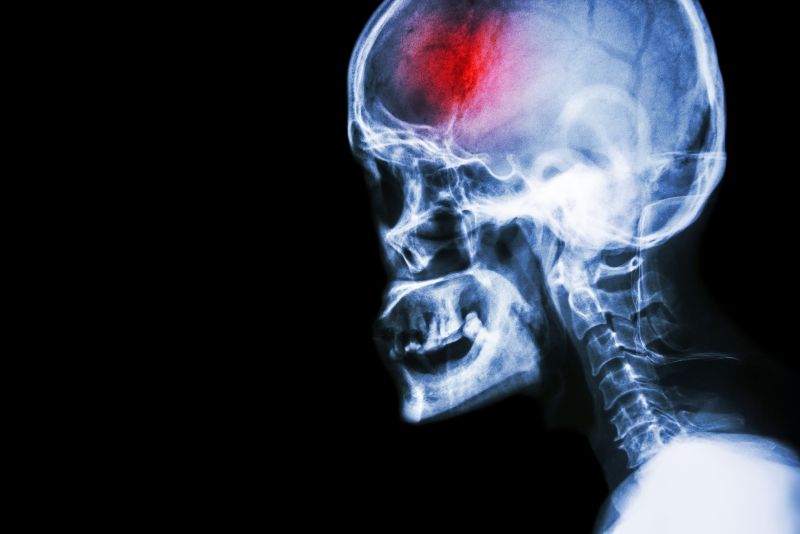
Every stroke that occurs is unique. Each is dependent on where in the brain the bleed or blockage occurs as well as how long it took for treatment to be administered. As mentioned before, there will most often be one side that is physically affected while the other side may remain physically unaffected. This is in contrast to a traumatic brain injury where both sides of the body may be affected equally or one more than the other.

The goal of rehabilitation after stroke is to teach you to become as independent as possible. The keystone to stroke rehabilitation is reteaching the brain to do the functions that have been affected by the stroke. The brain has an incredible ability to retrain a different area of the brain to take over the functions of the brain that have been lost due to the stroke. This is called neuroplasticity. “Neuro” refers to the brain cells and “plasticity” refers to the pliable nature of different brain cells to take over lost functions. With rehabilitation, brain cells regenerate, re-establish, and rearrange the needed brain circuits to resume lost functions despite the original cells and pathways having been damaged by the stroke. The brain effectively compensates for the dead or damaged brain cells. In instances where it cannot establish these new connections, rehabilitation works to teach the brain and body to compensate for the disabilities that occur due to the stroke.
Starting rehabilitation as early as possible is important to receive the most benefit. Once you are medically stable in the hospital, rehabilitation may begin as early as 48 hours after a stroke. Once you are discharged from the hospital then regular rehabilitation should continue either at home or at a clinic that specializes in stroke rehabilitation. Because repetition and intense practice is important in neuroplasticity, frequently repeated physical therapy sessions that focus on specific skills that are tailored to each patient’s individual deficits, as well as repeated practice of learned skills is very important. 45 minutes of therapy at least 2-5 times a week, depending on the patient’s goals and individual circumstances, is recommended and shown to be required to make measurable gains in rehabilitation. Although rehabilitation can be effective even years after a stroke, the most notable gains in rehabilitation are made early on in the rehabilitation process so physical therapy should start as soon as possible and be a regular part of the stroke recovery process.
As mentioned, each stroke presentation is unique. Your physical therapist will do an initial assessment of your individual problems and determine what needs to be addressed in your situation and what requires the most attention. They will inquire about your goals regarding returning to your activities of daily living. Working through the physical loss of strength and sensation on one side of your body may also be complicated by other stroke-induced impairments such as visual losses, as well as the ability to understand instructions and the ability to express one’s self (receptive and/or expressive aphasia) or actual difficulty speaking (dysphasia). Apraxia may also be present; this refers to losing the ability to carry out a learned purposeful movement or being unable to plan the steps involved in completing a complex task and doing them in the proper sequence, such as getting out of bed or making a cup of coffee.
Working in conjunction with other rehabilitation professionals such as speech pathologists and occupational therapists will be important in addressing all impairments simultaneously.
Proprioception and Balance
Simply put, proprioception, or kinesthesia, is the ability to know where your joint or limb is in space without looking at it. Proprioception is how we sense the position and movement of our body including our ability to balance.
A large part of stroke rehabilitation will be focused on proprioception and balance. Because one side of the body is affected during a stroke, proprioception and balance are usually severely compromised. Depending on where the stroke occurs in the brain (some areas are more involved in balance) and also depending on the severity of the stroke some patients will have trouble even sitting without losing their balance after a stroke. Others will be ok when sitting but are unable to stand or walk without losing their balance. Your physical therapist will work closely with you to gain the ability to sit, stand and walk, depending on your level of impairment.
Transfers
Transferring from one surface to another can be very difficult after a stroke when one side of your body is not functioning as it used to. Because getting in and out of bed, on and off a chair, on and off the toilet, in and out of the shower/bath and in and out of a car are all important tasks for daily living, your physical therapist will focus on gaining the needed strength and balance to master these tasks as soon as possible.
Strength and Range of Motion
After a stroke one side of the body is affected in its ability to voluntarily move, while the other side of the body may be completely normal. Depending on the severity and location of the stroke the muscles on the affected side may be completely paralysed (flaccid) or they may continue to have some movement available. The upper extremity (shoulder, arm and hand) is generally more adversely affected than the lower extremity (hip, leg and foot). It should be noted that even though initially the upper or lower limb on the affected side may be flaccid, often some movement will return over time with rehabilitation due to neuroplasticity. Some muscles, however, may be permanently paralysed or may not gain enough movement to be used for any purposeful function. Early rehabilitation is important to encourage activation of the muscles and promote neuroplasticity. Your physical therapist will assess the movement of your affected side and work to gain as much motion and strength as possible in any active muscles.
The goal of strengthening is to work towards enough strength and control in order for you to use your affected side as much as you can for activities of daily living, even if it is not as functional as it was prior to your stroke.
Gait
Returning to walking is the ultimate goal for most clients who have had a stroke. Fortunately, many can and will achieve this goal. In order to regain the ability to walk, the lower limb on your affected side will require enough strength, range of motion and control (proprioception) to support your body. In addition, you will require adequate standing and moving (dynamic) balance to achieve the skill of walking. Many patients who have had strokes but are able to walk will require a cane or walker which assists with their balance when on their feet. Your physical therapist will assess your skills and determine if and when working on the skill of walking is appropriate. Your therapist may use a form of biofeedback that helps you see or hear stimuli (rhythmic auditory stimuli) in conjunction with your movement in order to help you improve your walking pattern and cadence.
It is important for individuals to maintain as much independence as possible so your physical therapist will strive towards the goal of ambulation (walking) whenever possible. In cases where ambulation is not feasible then your physical therapist will assist in teaching you how to mobilize in a wheelchair on your own.
Other modalities
Stroke rehabilitation research is ongoing worldwide and new types of treatments are continually being tested for their efficacy. We know for sure that in order to encourage neuroplasticity, regular and ongoing rehabilitation which repeats meaningful tasks and addresses the specific deficits of each patient, including working towards doing functional activities (doing activities that one would do in daily life) is effective. Essentially rehabilitation in this regard is in line with how we would learn any new skill, such as a tennis serve or writing a new language; we would practice repeatedly and regularly the actual skills that are involved in the new task until we can put the skills together into the desired task. There are many types of modalities or treatments that may be trialled within your physical therapy sessions to assist in maximizing the skills gained. For example:
Mirrors: mirrors can be useful to help clients visualize their deficits and assist with proprioception, balance and ambulation. In a special type of mirror therapy your physical therapist may place the mirror between your limbs and cover up your affected limb so that when you move your strong side, it appears to your brain that your weaker side is moving. This may be an effective way to ‘trick’ the brain into thinking that it is moving the weaker side. This can assist in encouraging the weaker side to move on its own.
Constraint Therapy: during this type of therapy the strong side is actually immobilized so that the affected side is forced to do the work.
Bracing: some forms of standard or customized bracing may be used to assist the upper limb and hand as well as the weakness in the foot.
Treadmill Walking: at certain stages of rehabilitation a treadmill can be very effective in retraining ambulation. Depending on your level of function your therapist may choose to use the treadmill with or without a brace which helps to hold you up and support your body weight. Robotic-type electromechanical devices may be used if available to encourage the walking motion.
Visualization: encouraging a mental image of the task at hand is a very effective way to re-teach the affected limb. Your therapist may encourage you to shut your eyes and visualize several times your affected limb doing the task well, and then once you can do this, they will ask you to try doing the task with your affected side.
Virtual reality training: although not widely available, some clinics or therapists may have access to virtual reality technologies which may be useful in rehabilitation.
Aerobic training: for patients who maintain a high level of their functional abilities aerobic training can be incorporated in terms of treadmill training, cycling, or aquatic therapy.
Cycling: for patients who maintain a high level of their functional abilities, cycling may be used as a form of coordination and aerobic training.
Aquatic therapy: for patients who maintain a high level of their functional abilities aquatic therapy can be used for coordination, strength, gait and aerobic training.
Tai Chi: for patients who maintain a high level of their functional abilities tai chi is an effective form of training for balance and proprioception
Force platform training: if available, the feedback from a force plate which measures weight bearing can be used to assist balance and proprioception training
Interdisciplinary Team Review
A stroke affects the whole person; depending on the severity it can physically affect both your upper and lower limbs, your cognition, your vision, your speech and your emotional and mental health. As such, it is important to work with a full multidisciplinary team in order to best treat and manage all affected aspects. Your team may include your doctor, your physical therapist, a speech pathologist, an occupational therapist, a dietician, a psychologist, a social worker, and other health care professionals. Together this team of professionals can address your deficits as a whole and work together to provide you with the most effective treatment to maximize your overall abilities.
STAR Physical Therapy provides services for physical therapy in Fairport and Rochester.
 Other tests
Other tests
 A stroke is a serious medical emergency that requires immediate action in order to achieve the best eventual outcomes. Early medical intervention, as well as early, consistent and ongoing rehabilitation will positively affect your long term capabilities. Physical therapy services at STAR Physical Therapy can assist you to recover from your stroke and regain your maximum potential.
A stroke is a serious medical emergency that requires immediate action in order to achieve the best eventual outcomes. Early medical intervention, as well as early, consistent and ongoing rehabilitation will positively affect your long term capabilities. Physical therapy services at STAR Physical Therapy can assist you to recover from your stroke and regain your maximum potential.