What will my recovery be like?
Generally a physical therapist will see you the day after surgery to begin your rehabilitation program while you are in the hospital. Your therapist will make sure you are safe getting in and out of bed and moving about in your room with your sling on. Next they will prescribe specific range of motion exercises for you that you will begin immediately as long as your surgeon allows it. Your therapist will teach you how to remove your sling for your exercises and also how to put it back on after you have completed your exercises. The sling should be worn at all times except during showering and while performing rehabilitation exercises.
When the immobilizer is removed following surgery, you will experience some pain when you start to move your shoulder, wrist, elbow and forearm, and this is normal. This pain is from not using the joints very well prior to the surgery and also from the surgical process itself. The pain you feel should only be mild to moderate and any sharp or severe pain should be heeded. In addition, the muscles in your arm may already appear small and atrophied. Again, this is normal; once your strength beings to return your arm will start to look more normal again.
Simple finger, hand and wrist movements, as well as elbow and neck range of motion exercises will be prescribed to ensure you regain motion in these joints. For your shoulder, generally pendular exercises are prescribed along with passive range of motion exercises that encourage shoulder elevation (raising in front) as well as gentle external rotation. Pendular exercises assist with pain, help to maintain some shoulder range of motion, and assist in preventing unwanted scar tissue forming in the joint. These exercises are performed by leaning forward or to the side, letting the arm hang clear of the chest, and then initiating movement with your trunk so that the dangling limb passively and gently moves. This action provides some traction to the glenohumeral joint, which aids in pain relief, and also assists the shoulder into a relatively elevated motion (in relation to the trunk.) It is important that the pendular activity is done as passively as possible without initiating motion from the shoulder muscles.
The exercise should be similar to a weighted pendulum that randomly swings on the end of a piece of string. Icing your shoulder will be encouraged after your exercises as well as several other times during the day.
In cases where the reverse shoulder arthroplasty has been done as a revision to a traditionally replaced shoulder, or where the surgical approach has included cutting through the deltoid muscle, the initiation of early exercises will need to be delayed to allow a prolonged period of healing before putting the shoulder under any stress. In these cases your surgeon and therapist will direct you in regards to which exercises are initially allowed, and which should be avoided. In all reverse shoulder replacement cases the specific post-surgical protocol of your surgeon should be strictly adhered to. Each surgeon has their own protocol based on personal preference and experience, as well as surgical technique.
No matter which post-surgical protocol is followed, protecting the new joint is of particular importance after a reverse shoulder arthroplasty. Due to the biomechanics of a reverse arthroplasty there is a higher risk of shoulder dislocation following a reverse shoulder arthroplasty versus a traditional shoulder replacement. Unlike a traditional shoulder replacement, which is more likely to dislocate with the arm in abduction and external rotation, the reverse shoulder replacement is at risk of dislocation during isolated extension as well as the combined movements of extension, internal rotation, and adduction. Your therapist will review these movement precautions with you and you should refrain from putting your shoulder in any of these positions on their own or in combination for a minimum of 12 weeks post-surgically. Activities involving these positions, such as tucking in one’s shirt or performing personal hygiene of the back passage, are simple activities but can lead to dislocation so must be strictly avoided. It can be helpful in respecting these precautions by remembering that you should always be able to see the elbow on your surgical side during all activities with that arm.
Once you are managing your exercises well in the hospital, you are independent in doing most activities to care for yourself, and when your surgeon feels it is appropriate, you will be sent home. You will need to continue an extensive rehabilitation program once you are discharged from the hospital. In some cases, a physical therapist or occupational therapist may visit your home to check to see that you are safely getting around in your home and managing your everyday tasks with your arm in your sling. Your therapist may also review and assist you with your exercises at this time. If it is particularly difficult for you to get out of your home to attend physical therapy at STAR Physical Therapy then a physical therapist may continue to visit you at your home for several treatments in order to review and advance your exercises. As soon as you are able, however, it is best for you to attend rehabilitation at STAR Physical Therapy as there are several more modalities as well as exercise equipment that can be used in the clinic versus at home, which can expedite your recovery.
As an initial goal of rehabilitation your physical therapist at STAR Physical Therapy will focus on relieving your pain and decreasing any swelling that may be lingering from the surgery. We may use modalities such as heat, ice, or electrical current to assist with decreasing any pain or swelling you have around the shoulder, anywhere along the arm, or into the hand. Due to some of the muscles of the neck and upper back connecting to the shoulder, you may also have pain in these regions, which we can treat in order to make movement of your entire upper body easier. We may also use massage or mobilizations for the neck, upper back, shoulder, elbow, forearm, or wrist to improve circulation and assist with any pain that may be present.
Due to the ongoing possibility of dislocation with a reverse shoulder arthroplasty, once you have begun therapy at STAR Physical Therapy your therapist will review the shoulder motion precautions of shoulder extension, internal rotation, and adduction that will strictly need to be avoided for the first 12 weeks post-surgically, or until your surgeon advises you otherwise.
The next part of our treatment will focus on regaining the range of motion, strength, and dexterity in your wrist, hand, elbow, and shoulder. Your physical therapist at STAR Physical Therapy will prescribe a series of stretching and strengthening exercises that you will practice in the clinic and also learn to do as part of your home exercise program. These exercises may include the use of rehabilitation equipment such as pulleys and poles for range of motion exercises, and light weights or exercise band for resistance work of your upper limb. The shoulder joint is the upper limb’s link to the rest of the body so it needs to be strong and well controlled for the limb and hand to work well. Exercises following a reverse shoulder arthroplasty will focus initially on gaining passive then active-assisted range of motion, while initiating some early light strengthening of the deltoid muscle as well as the other muscles around the shoulder blade that support the shoulder girdle. All exercises should be done with pristine technique as to not compromise the new shoulder joint. Your shoulder precautions should strictly be abided by and, in addition, once you have more range of movement you should be careful not to support your body weight at all with your surgical limb (ie: pushing off of a chair to get up or pushing a door open) nor lift much more than the weight of a coffee cup until your therapist clears you to do so.
Your physical therapist will be crucial in providing feedback during your exercises in order to ensure they are being done properly and safely. As time and range of motion progress, strengthening will become the major focus and will be advanced so that light weights or elastic bands are used and endurance of the muscles is improved. Your therapist will monitor your progress and advance your exercises as your shoulder can tolerate them. Along with more advanced strengthening exercises active range of motion of the shoulder will be encouraged in order to assist with strengthening and control of the entire shoulder girdle.
Proprioception is the ability to know where your body is without looking at it. As a result of any injury or surgery, this ability declines in function. A period of immobility adds to this decline. Although your arm and shoulder girdle are not traditionally thought of as weight-bearing parts of the body, even an activity such as assisting yourself with your arms to get out of a chair or pulling a plate from a cupboard requires weight to be put through your shoulder girdle and for your body to be proprioceptively aware of your limb.
The proprioceptive control of the scapula on the rib cage (scapulothoracic motion) is especially important in being able to use your shoulder girdle and upper limb effectively without causing further injury. For this reason, your physical therapist will teach you how to properly control your scapula during your rehabilitation exercises as well as during everyday activities. Your physical therapist will also remind you about maintaining good shoulder posture even when sitting or using your upper limb in activities below shoulder height, such as working on the computer. Rounded shoulders in this position crowds the shoulder joint and can lead to shoulder impingement and pain. Regaining proprioception of the shoulder girdle and upper limb can require concentrated work, and most people have not previously needed to focus so intently on such controlled motions of this joint. The concentrated effort of shoulder rehabilitation however, has a substantial reward; good scapulothoracic control is the key to regaining maximum shoulder girdle control and thus improved shoulder functioning while avoiding future shoulder pain.
Proprioceptive exercises might include activities such as rolling a ball on a surface with your hand, holding a weight up while moving your shoulder, or push-ups on an unstable surface. Advanced exercises may include activities such as ball throwing or catching. As often as possible, exercises will be incorporated that mimic your everyday activities such as grooming yourself and getting dressed, in addition to those activities that simulate your work or hobbies.
As rehabilitation advances most patients with a reverse shoulder replacement will be able to lift their arm with little or no pain. Some patients, however, may take many months to recover to this stage. It should be noted that with all reverse shoulder arthroplasty surgeries the return of full shoulder elevation or external rotation is not expected. A goal of approximately 105 degrees elevation should be anticipated. The amount of external rotation following surgery will be dependent on the state of the rotator cuff muscles prior to surgery. Despite the relative loss of range of motion, for most patients the ability to achieve this range of motion without pain offers a very functional shoulder, particularly in comparison to the shoulder’s pre-surgical status.
Generally rehabilitation at STAR Physical Therapy after reverse shoulder arthroplasty goes smoothly, however, if during rehabilitation your pain continues longer than it should or therapy is not progressing as your physical therapist would expect, we will ask you to follow-up with your surgeon or doctor to confirm that the shoulder is tolerating the rehabilitation well and to ensure that there are no hardware issues that may be impeding your recovery.
STAR Physical Therapy provides services for physical therapy in Fairport and Rochester.
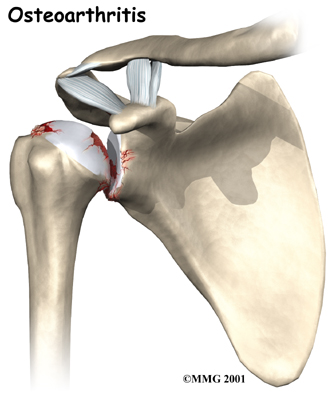
 Shoulder joint replacement surgery (also called shoulder arthroplasty) can effectively ease pain from shoulder arthritis. Most people experience improved shoulder function after this surgery. Unfortunately certain patients are not candidates for a traditional joint replacement of the shoulder because they lack the muscle function necessary to stabilize the joint. A different type of shoulder replacement, called a reverse shoulder replacement, may be available for many of these patients and provide pain relief as well as a stable functioning shoulder that is adequate for their daily needs.
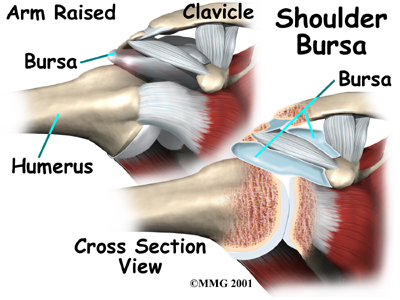
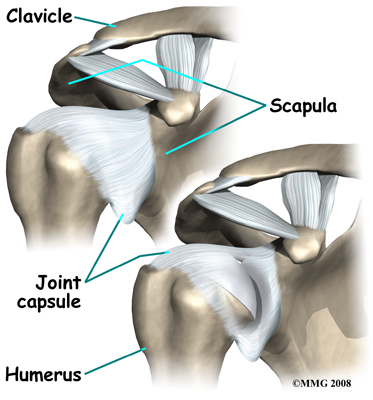
Shoulder joint replacement surgery (also called shoulder arthroplasty) can effectively ease pain from shoulder arthritis. Most people experience improved shoulder function after this surgery. Unfortunately certain patients are not candidates for a traditional joint replacement of the shoulder because they lack the muscle function necessary to stabilize the joint. A different type of shoulder replacement, called a reverse shoulder replacement, may be available for many of these patients and provide pain relief as well as a stable functioning shoulder that is adequate for their daily needs.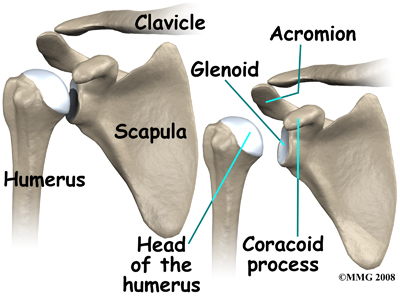 The shoulder is made up of three bones: the scapula (shoulder blade), the humerus (upper arm bone), and the clavicle (collarbone).
The shoulder is made up of three bones: the scapula (shoulder blade), the humerus (upper arm bone), and the clavicle (collarbone).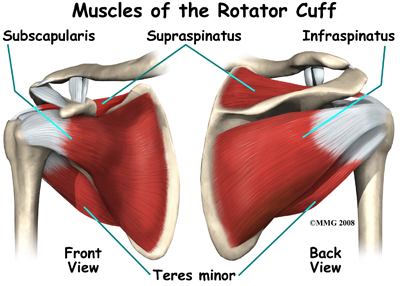
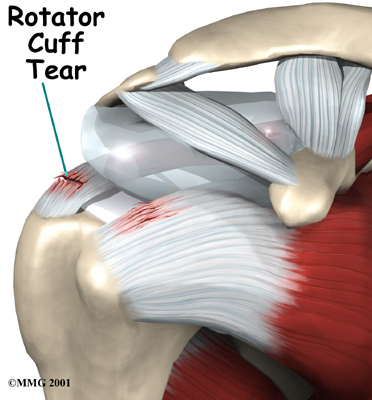 Surgery to repair a rotator cuff tear is fairly common in people who are middle aged or older. Small, medium and many large tears can be repaired either through arthroscopic or open surgical procedures. Most rotator cuff repairs are successful but in a portion of patients the torn tendon has become so degenerated that the tendon cannot be repaired. Unfortunately, many large tears that are untreated for a long time may retract which renders them unfixable.
Surgery to repair a rotator cuff tear is fairly common in people who are middle aged or older. Small, medium and many large tears can be repaired either through arthroscopic or open surgical procedures. Most rotator cuff repairs are successful but in a portion of patients the torn tendon has become so degenerated that the tendon cannot be repaired. Unfortunately, many large tears that are untreated for a long time may retract which renders them unfixable.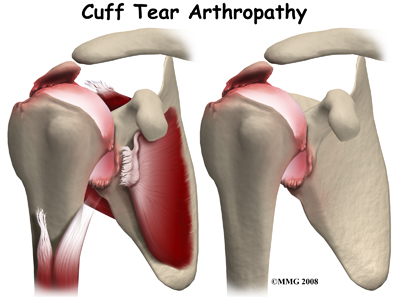 Cuff tear arthropathy is difficult to treat. The shoulder is weak and painful. Patients may not be able to raise the arm above shoulder level. Patients with this type of arthritis would seem to be good candidates for a shoulder replacement, but replacing the shoulder in the traditional fashion has not been successful.
Cuff tear arthropathy is difficult to treat. The shoulder is weak and painful. Patients may not be able to raise the arm above shoulder level. Patients with this type of arthritis would seem to be good candidates for a shoulder replacement, but replacing the shoulder in the traditional fashion has not been successful.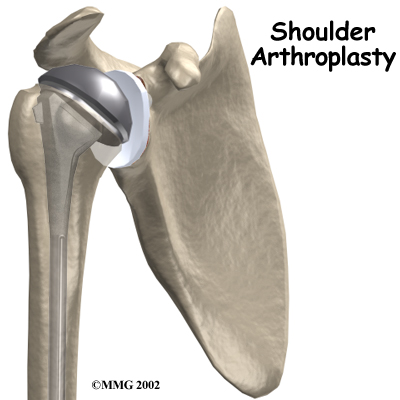
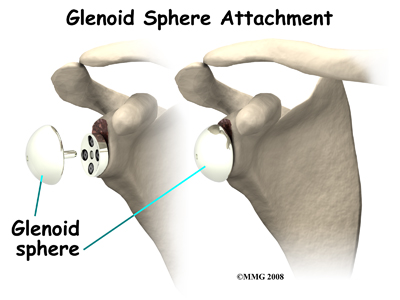
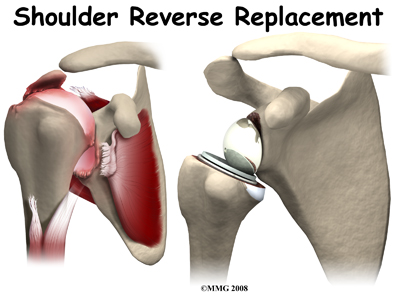
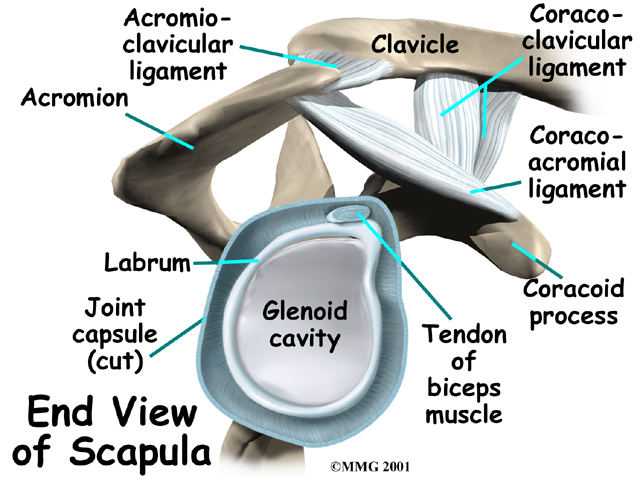
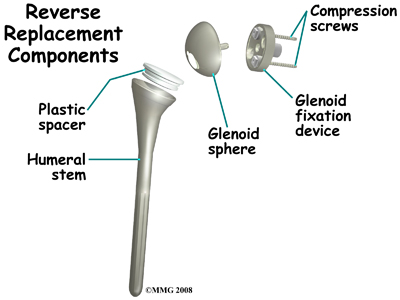 The reverse shoulder prosthesis (artificial joint) is made up of two parts. The humeral component replaces the humeral head, or the ball of the joint. The glenoid component replaces the socket of the shoulder, which is actually part of the scapula.
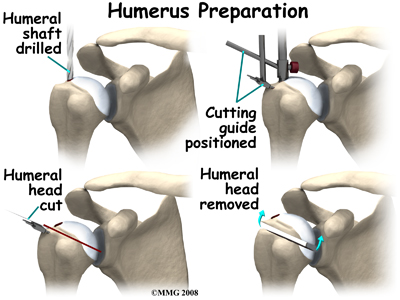
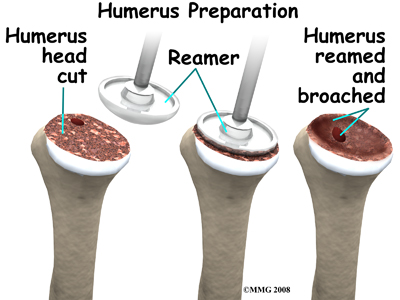
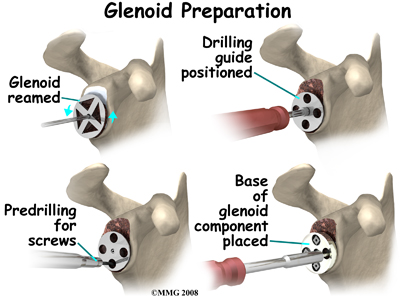
The reverse shoulder prosthesis (artificial joint) is made up of two parts. The humeral component replaces the humeral head, or the ball of the joint. The glenoid component replaces the socket of the shoulder, which is actually part of the scapula.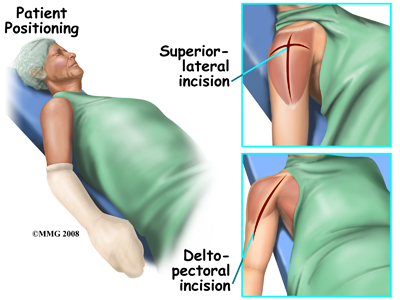 Shoulder replacement surgery is done through an incision on the front of your shoulder. This is called an anterior (deltopectoral) approach. For reverse shoulder replacements, especially for patients with multiple previous surgeries, a superior approach through the deltoid muscle may be used. No matter which approach is used, the surgeon cuts through the skin and then isolates the nerves and blood vessels and moves them to the side. The muscles are also moved to the side. If the deltoid requires cutting, a delay in your rehabilitation will be needed to allow the deltoid muscle to heal before putting stress through it.
Shoulder replacement surgery is done through an incision on the front of your shoulder. This is called an anterior (deltopectoral) approach. For reverse shoulder replacements, especially for patients with multiple previous surgeries, a superior approach through the deltoid muscle may be used. No matter which approach is used, the surgeon cuts through the skin and then isolates the nerves and blood vessels and moves them to the side. The muscles are also moved to the side. If the deltoid requires cutting, a delay in your rehabilitation will be needed to allow the deltoid muscle to heal before putting stress through it.