What treatment options are available?
Nonsurgical Treatment
In many cases, the shoulder can be reduced without surgery. This is called a closed reduction. Many health care professionals (especially those trained in emergency procedures) know how to manipulate the shoulder back into the socket. However, without the aid of a general anesthetic, this maneuver can be very painful.
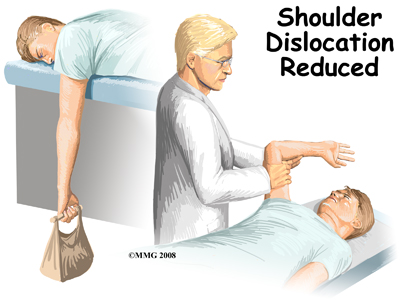 One simple technique used by health care professionals to reduce an anterior shoulder dislocation is done in the prone (face down) position. The injured arm is supported at the edge of the table. The arm is allowed to dangle over the edge of the table with a weight attached. As the shoulder muscles relax, the humeral head passively (on its own) slips back to its normal position. Unfortunately this may take several minutes.
One simple technique used by health care professionals to reduce an anterior shoulder dislocation is done in the prone (face down) position. The injured arm is supported at the edge of the table. The arm is allowed to dangle over the edge of the table with a weight attached. As the shoulder muscles relax, the humeral head passively (on its own) slips back to its normal position. Unfortunately this may take several minutes.
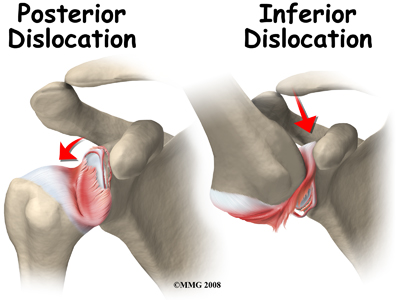
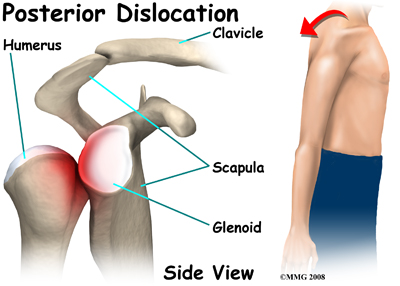
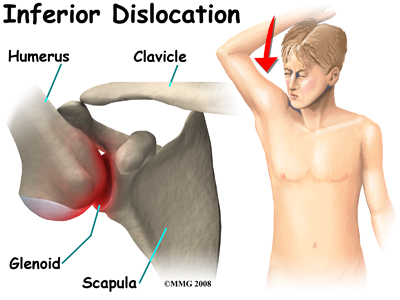
If passive positioning doesn't work for an anterior dislocation, then a general anesthetic is administered and traction is applied to the upper limb. The arm is held in a position of shoulder abduction while lateral (sideways) and backward pressure is applied to the head of the humerus. Posterior shoulder dislocation can be treated in a similar fashion. Under anesthesia, the shoulder is rotated outwardly and forward pressure is applied on the dislocated humeral head.
Some patients who have recurrent dislocations know how to pop their own joint back into place without help. When performed by a health care professional, the procedure is generally done in a timely manner in order to prevent further pain or soft tissue damage.
Functional outcome is also better if the dislocation is reduced early.
 Following closed reduction, X-rays are used to confirm correct placement of the humeral head in the glenoid cavity. After reduction, immobilization of the arm in a sling against the chest is usually recommended for several weeks up to a month. This period of immobilization gives the soft tissues a chance to heal.
Following closed reduction, X-rays are used to confirm correct placement of the humeral head in the glenoid cavity. After reduction, immobilization of the arm in a sling against the chest is usually recommended for several weeks up to a month. This period of immobilization gives the soft tissues a chance to heal.
As older adults are more at risk of developing a stiff or frozen shoulder, gentle range of motion exercises called Codman's or pendulum exercises may be prescribed for these individuals. These are usually done once or twice a day with the sling removed.
Recurrent dislocation is the most common complication after dislocation, especially in young people. Older adults are more likely to experience chronic pain and stiffness. When conservative care is unable to restore shoulder stability and normal function, then surgical intervention may be needed.
Nonsurgical Rehabilitation
All shoulder dislocations do not require surgery. Many dislocations, especially in middle or older age, can be treated non-surgically. Physical therapy at STAR Physical Therapy will assist you in restoring the normal function of your shoulder. Immediately following your dislocation, your shoulder will likely require a period of immobilization in a sling for 2-4 weeks. This immobilization is to assist in pain relief, and allow the soft tissue to heal. As mentioned above, in the middle age to older population, a shorter immobilization period avoids a potentially stiff shoulder, whereas in a younger population, the longer immobilization period allows scarring of the tissues to prevent a recurrence of the injury.
Initially, the treatment we provide at STAR Physical Therapy will be focused on relieving any pain and inflammation caused by the dislocation and reduction of your shoulder joint. We may use modalities such as ice, heat, ultrasound, or electrical current to assist with decreasing any pain or swelling you have. Due to some of the muscles of the neck and upper back connecting to the shoulder, you may also have pain in these regions and require treatment for these areas. Massage may be used for the neck, upper back, and non-painful areas of the shoulder to decrease pain. In addition, taping the shoulder during the initial stages of recovery may assist with pain relief by easing the tension placed on inflamed structures.
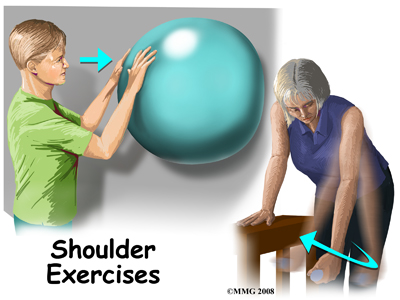
While you are immobilized simple finger movements, elbow and neck range of motion exercises should be performed. If your physical therapist or doctor has stated that your shoulder is at risk of becoming stiff, pendular (Codman) exercises (with the immobilizer removed), will also be encouraged. Pendular exercises assist with pain relief, help to maintain some shoulder range of motion, and assist in preventing unwanted scar tissue forming in the joint. These exercises are performed by leaning forward or to the side, letting the arm hang clear of the chest, and then initiating movement with your trunk so that the dangling limb passively and gently moves. This action provides some traction to the glenohumeral joint, which aids in pain relief, and also assists the shoulder into a relative elevated motion (in relation to the trunk.) It is important that the pendular activity is done as passively as possible without initiating motion from the shoulder muscles. The exercise should be similar to a weighted pendulum that randomly swings on the end of a piece of string.
At STAR Physical Therapy we highly recommend maintaining the rest of your body’s fitness with regular exercise even while your shoulder is immobilized. Cardiovascular fitness can be maintained with lower extremity fitness activities such as walking or using a stationary bike or stepper machine. None of these exercises should cause discomfort to your shoulder; if this occurs, discuss modifying the activity with your physical therapist.
The next part of our treatment will focus on regaining the range of motion, strength, and coordination in your shoulder. The desired outcome of rehabilitation after shoulder dislocation is a return to full function. For athletes, this means full participation in sports activities. Depending on how long you were immobilized, your age, as well as the severity of the injury, your arm may feel very weak and be limited in its range of motion once the immobilizer is removed. Shoulders that have not lost some range of movement after the period of immobilization are often suspicious for eventual recurrence of the dislocation.
In order to gain back your range of motion, strength, and function of your shoulder your physical therapist at STAR Physical Therapy will prescribe a series of stretching and strengthening exercises that you will practice in the clinic and also learn to do as part of a home exercise program. These exercises may include the use of rehabilitation equipment such as pulleys and poles for range of motion exercises, and light weights or Theraband for resistance work of your upper limb. As mentioned previously, the shoulder joint is very mobile, but anatomically not very stable and relies heavily on the strength and coordinated function of the muscles around it to maintain its stability and avoid dislocation. The rotator cuff muscles that assist to hold the shoulder joint in the socket are particularly important so will be targeted with rotational resistance activities of the shoulder in different ranges of motion. Adequate strength and endurance in the rotator cuff muscles throughout a variety of ranges of motion is needed to ensure full functioning of the shoulder. An upper body bike may be useful in the early stages of rehabilitation to improve range of motion and encourage coordinated movement of the entire upper limb.
If necessary, your physical therapist will mobilize your shoulder joint. This hands-on technique encourages your shoulder to move gradually into its normal range of motion. Fortunately, gaining range of motion and strength once the shoulder is no longer immobilized occurs fairly quickly. You will notice improvements in the functioning of your shoulder even after just a few treatments with your physical therapist at STAR Physical Therapy.
As a result of any injury, the receptors in your joints and ligaments that assist with proprioception (the ability to know where your body is without looking at it) decline in function. This is particularly true when the stability of a joint has been disrupted. A period of immobility will add to the decline of these receptors. Although your arm and shoulder girdle are not traditionally thought of as weight-bearing parts of the body, an activity such as assisting yourself with your arms to get out of a chair, pulling a glass from a cupboard, or even shaving requires weight to be put through or lifted by your shoulder girdle and for your body to be proprioceptively aware of your limb. If you are an athlete, then proprioception of your upper extremity is paramount in returning you to your sport after a shoulder dislocation. Overhead sports such as swimming, or volleyball require even more precise control of the shoulder joint and girdle in order to fully return to your sport.
Controlled scapulothoracic motion is particularly essential when using your limb near or above shoulder height and especially during rapid arm movements such as throwing. By ensuring proprioceptive control of the scapula on the rib cage (scapulothoracic motion) you decrease the risk of further injury to the shoulder and the risk of another dislocation. For this reason, your physical therapist will teach you how to properly control your scapula during your rehabilitation exercises but will also educate you on transferring this control to your everyday activities. As you improve with being able to control the shoulder girdle your physical therapist will introduce more difficult dynamic exercises for your shoulder including exercises that simulate your everyday activities, or if you are an athlete, those shoulder motions that simulate your sport. Simple proprioceptive exercises might include activities such as rolling a ball on a surface with your hand, holding a weight up overhead while moving your shoulder, or pushups on an unstable surface. Advanced exercises may include activities such as reaching and lowering a weight, ball throwing, catching overhead, or a simulated swimming stroke or overhead spike. Your physical therapist will tailor your proprioception exercises to best address your direction of instability, your level of ability, and your return to function goal.
No matter which direction your shoulder has dislocated gaining scapulothoracic and glenohumeral control particularly during dynamic overhead motions and weight bearing activities is paramount in returning you to your full activities. If these advanced exercises cannot be mastered without pain or a feeling of apprehension, it is often reason for a surgical intervention to be considered and your physical therapist will liaise with your surgeon if this is the case. Unfortunately, regaining proprioception of the shoulder girdle and upper limb requires concentrated and determined work, and most people have not previously needed to focus so intently on such controlled motions of their shoulder blade and arm. The concentrated effort, however, has a substantial reward, as good scapulothoracic control is the key to regaining maximum shoulder function after a dislocation, preventing a second dislocation, and avoiding secondary pain from shoulder impingement in the future. Whether treating a shoulder dislocation non-surgically or surgically, scapulothoracic control is an essential part of your physical therapy rehabilitation.
Finally, as part of your shoulder rehabilitation, your physical therapist will also remind you about maintaining good shoulder posture at all times even when just sitting or using your upper limb in activities below shoulder height, such as working on the computer. Rounded shoulders in any position crowds the shoulder joint and can lead to shoulder impingement and pain as you recover from your dislocation.
Rehabilitation after a shoulder dislocation responds very well to the physical therapy we provide at STAR Physical Therapy. As a general guide you can return to you will be able to return to your full sporting activities as long as there is no pain or recurrent swelling, when your muscles are back to nearly their full strength and control, and you aren't having problems with the shoulder popping out of the joint.
STAR Physical Therapy provides services for physical therapy in Fairport and Rochester.
 Welcome to STAR Physical Therapy's resource about shoulder dislocations.
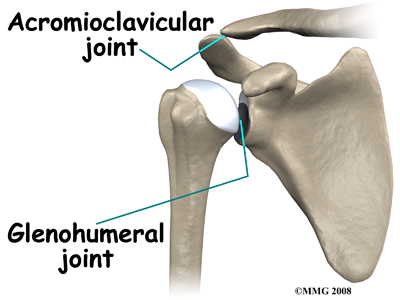
Welcome to STAR Physical Therapy's resource about shoulder dislocations.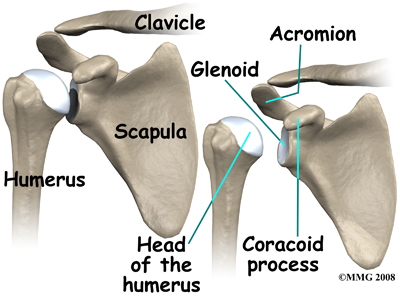 The shoulder has a unique and complex anatomy that allows range of motion and coordination needed for reaching, lifting, throwing, and many other movements. Understanding the anatomical structures discussed will help you understand why your shoulder dislocated.
The shoulder has a unique and complex anatomy that allows range of motion and coordination needed for reaching, lifting, throwing, and many other movements. Understanding the anatomical structures discussed will help you understand why your shoulder dislocated.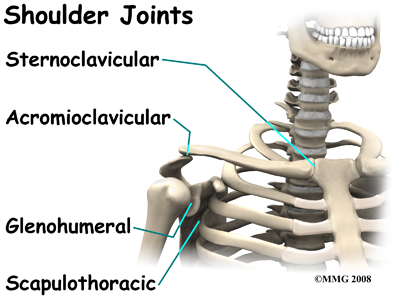
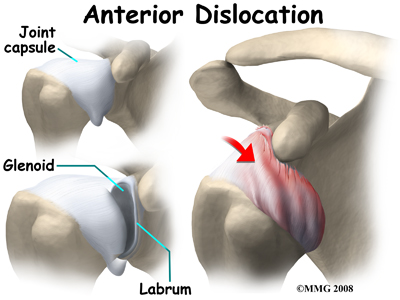
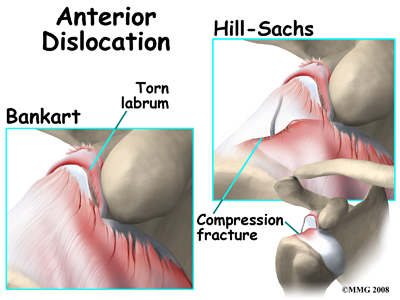
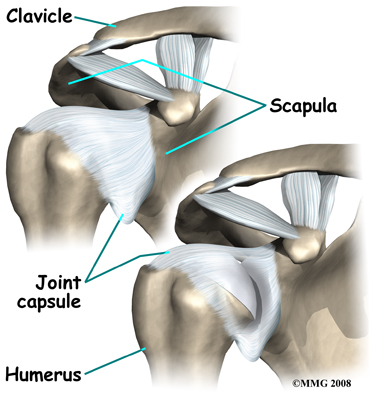 There are several important ligaments in the shoulder. Ligaments are soft tissue structures that connect bones to bones. A joint capsule is a watertight sac that surrounds a joint. In the shoulder, the joint capsule is formed by a group of ligaments that connect the humerus to the glenoid. These ligaments are the main source of stability for the shoulder; they help hold the shoulder in place and keep it from dislocating.
There are several important ligaments in the shoulder. Ligaments are soft tissue structures that connect bones to bones. A joint capsule is a watertight sac that surrounds a joint. In the shoulder, the joint capsule is formed by a group of ligaments that connect the humerus to the glenoid. These ligaments are the main source of stability for the shoulder; they help hold the shoulder in place and keep it from dislocating.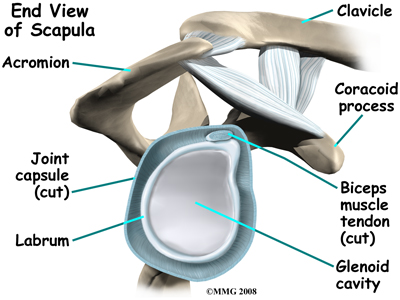
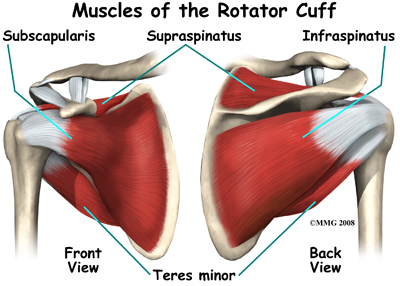 The tendons of the rotator cuff are the next layer in the shoulder joint. Four rotator cuff tendons connect the deepest layer of muscles to the humerus. This group of muscles attaches from the shoulder blade to the humerus. These muscles help raise the arm from the side and rotate the shoulder in the many directions. They are extremely important muscles to the shoulder and are involved in many day-to-day activities. The rotator cuff muscles and tendons are extremely important in assisting glenohumeral joint stability because they help hold the humeral head in the shallow glenoid socket.
The tendons of the rotator cuff are the next layer in the shoulder joint. Four rotator cuff tendons connect the deepest layer of muscles to the humerus. This group of muscles attaches from the shoulder blade to the humerus. These muscles help raise the arm from the side and rotate the shoulder in the many directions. They are extremely important muscles to the shoulder and are involved in many day-to-day activities. The rotator cuff muscles and tendons are extremely important in assisting glenohumeral joint stability because they help hold the humeral head in the shallow glenoid socket.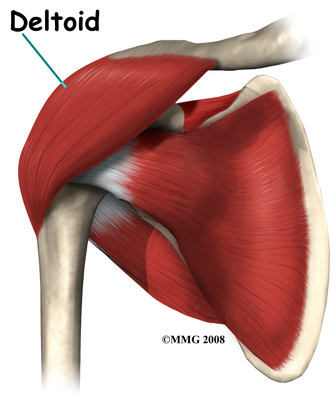
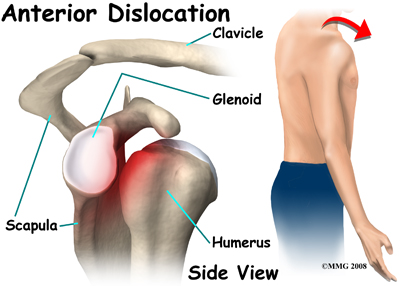
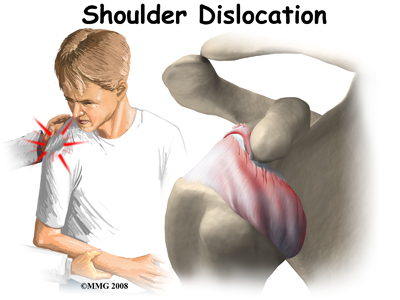
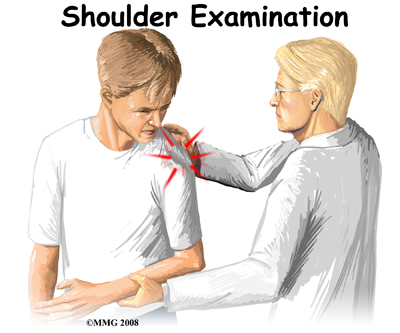 The history and physical examination are probably the most important tools used to diagnose a shoulder dislocation. The history of your injury is especially important. If the shoulder remains out of joint, the diagnosis is usually blatant. If, however, the joint has spontaneously reduced after the injury, the diagnosis of a shoulder dislocation having occurred may be less conspicuous.
The history and physical examination are probably the most important tools used to diagnose a shoulder dislocation. The history of your injury is especially important. If the shoulder remains out of joint, the diagnosis is usually blatant. If, however, the joint has spontaneously reduced after the injury, the diagnosis of a shoulder dislocation having occurred may be less conspicuous. 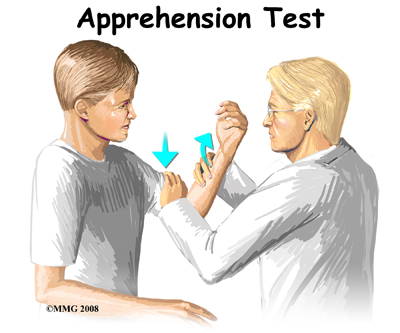 Range of motion, strength, and sensation will be tested if possible. Any there are any changes or loss of sensation this may point to nerve damage that has occurred as a result of the dislocation. Your physical therapist may also check the pulses in your arm in order to detect the possibility of vascular complications.
Range of motion, strength, and sensation will be tested if possible. Any there are any changes or loss of sensation this may point to nerve damage that has occurred as a result of the dislocation. Your physical therapist may also check the pulses in your arm in order to detect the possibility of vascular complications.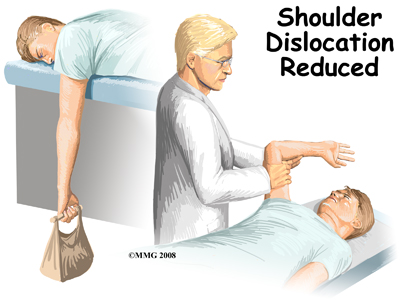 One simple technique used by health care professionals to reduce an anterior shoulder dislocation is done in the prone (face down) position. The injured arm is supported at the edge of the table. The arm is allowed to dangle over the edge of the table with a weight attached. As the shoulder muscles relax, the humeral head passively (on its own) slips back to its normal position. Unfortunately this may take several minutes.
One simple technique used by health care professionals to reduce an anterior shoulder dislocation is done in the prone (face down) position. The injured arm is supported at the edge of the table. The arm is allowed to dangle over the edge of the table with a weight attached. As the shoulder muscles relax, the humeral head passively (on its own) slips back to its normal position. Unfortunately this may take several minutes.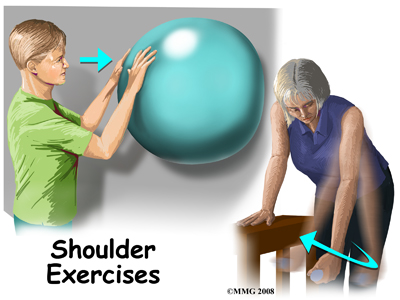 Following closed reduction, X-rays are used to confirm correct placement of the humeral head in the glenoid cavity. After reduction, immobilization of the arm in a sling against the chest is usually recommended for several weeks up to a month. This period of immobilization gives the soft tissues a chance to heal.
Following closed reduction, X-rays are used to confirm correct placement of the humeral head in the glenoid cavity. After reduction, immobilization of the arm in a sling against the chest is usually recommended for several weeks up to a month. This period of immobilization gives the soft tissues a chance to heal.