What should I expect during treatment?
Physical therapy at STAR Physical Therapy can be very useful for patients suffering from osteonecrosis of the shoulder, particularly if treatment is begun in the early stages of the disease.
The first goal of our treatment at STAR Physical Therapy is to reduce pain and any inflammation around the shoulder. The use of ice, heat, ultrasound, and other electrical modalities can be very useful as you begin your therapy. Your therapist may also use massage around the shoulder, neck or into the arm, which can help to ease pain and encourage blood flow to the affected area. Gentle mobilizations of the shoulder joint can also be helpful to ease any muscle spasm or pain.
While your therapist is trying to reduce the pain in your shoulder and encourage early healing, they may ask you to avoid lifting your arm overhead or away from your body against resistance. They will also encourage you to avoid lifting or holding anything heavy. They may even give you a weight restriction (i.e., don't lift anything more than two to five pounds or 1-2 kilograms). This restriction will include avoiding some everyday functional activities, such as putting away heavy groceries.
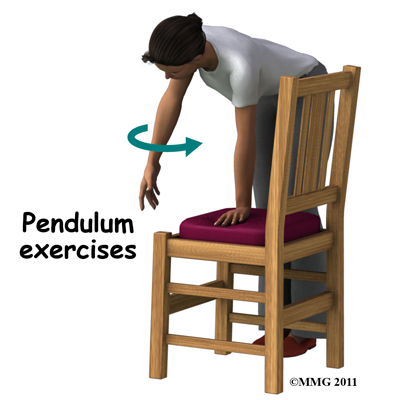 As soon as possible your therapist will begin to work on regaining your shoulder’s motion. They will teach you exercises that you can do yourself to assist with range of motion, which may include the use of sticks or pulleys to help raise the shoulder passively or your therapist may encourage you to partially use the muscles on your affected side (with the assistance of your good side) without causing discomfort. Doing pendular exercises can also help to maintain some shoulder range of motion and assist with pain at this stage. Pendular exercises are performed by leaning forward or to the side, letting the arm hang clear of the chest, and then initiating movement with your trunk so that the dangling limb passively and gently moves. This action provides some traction to the shoulder joint, which aids in pain relief, and also assists the shoulder into a relatively elevated position (in relation to the trunk.) It is important that the pendular activity is done as passively as possible without initiating motion
As soon as possible your therapist will begin to work on regaining your shoulder’s motion. They will teach you exercises that you can do yourself to assist with range of motion, which may include the use of sticks or pulleys to help raise the shoulder passively or your therapist may encourage you to partially use the muscles on your affected side (with the assistance of your good side) without causing discomfort. Doing pendular exercises can also help to maintain some shoulder range of motion and assist with pain at this stage. Pendular exercises are performed by leaning forward or to the side, letting the arm hang clear of the chest, and then initiating movement with your trunk so that the dangling limb passively and gently moves. This action provides some traction to the shoulder joint, which aids in pain relief, and also assists the shoulder into a relatively elevated position (in relation to the trunk.) It is important that the pendular activity is done as passively as possible without initiating motion
from the shoulder muscles. The exercise should look similar to a weighted pendulum that randomly swings gently on the end of a piece of string.
Maintaining your neck range of motion is also very important when your shoulder is not moving well, so your therapist will also prescribe exercises to ensure you can move your neck well for all your daily activities, and that you don’t end up with a stiff neck along with your painful shoulder.
Your therapist may also manually assist your range of motion by stretching or mobilizing your shoulder. Your therapist may need to work on any part of the shoulder joint including the glenohumeral joint, the joint between the shoulder blade and the thorax (scapulothoracic joint), or even the joints where your collarbone joins the trunk and the shoulder (sternoclavicular and acromioclavicular joints.) Your physical therapist will passively move these joints into their available ranges of motion while you try to relax the muscles of your shoulder completely.
Next, once your pain is under control and your shoulder range of movement is improving, your therapist will focus on strengthening exercises. Your therapist will start by prescribing simple strengthening exercises that only involve isometric strengthening. Isometric strengthening exercises are done by tightening your muscles without actually moving the associated joint. Isometric exercises work the muscles without straining the injured or painful shoulder. Your physical therapist will teach you how to use your other hand or a wall for resistance while you flex and tighten your muscles, creating an isometric contraction of the shoulder muscles. Your therapist will then progress your exercises so that you are strengthening the muscles through their available ranges of movement, as you are able. More advanced exercises will involve the use of light weights or exercise band to add resistance for your upper limb.
As a result of any injury, the receptors in your joints and ligaments that assist with proprioception (your joint’s sense of position) decline in function. A period of decreased mobility will add to this decline. Proprioception is particularly important when any joint is bearing weight. Although your arm and shoulder girdle are not traditionally thought of as weight-bearing parts of the body, even an activity such as assisting yourself with your arms to get out of a chair or pulling a glass from a cupboard requires weight to be put through or lifted by your shoulder girdle and for your body to be proprioceptively aware of your limb.
Proprioceptive exercises might include activities such as rolling a ball on a surface with your hand, lying on your back while holding and moving a weight up overhead, or pushups on an unstable surface. Advanced exercises may include activities such as ball throwing or catching overhead once you have regained that range of motion.
The proprioceptive control of the shoulder blade (scapula) on the rib cage (scapulothoracic motion) is especially important in being able to use your shoulder girdle and upper limb effectively without causing further injury. Normal scapulothoracic motion is particularly essential once you are able to use your limb near or above shoulder height. For this reason, your physical therapist will teach you how to properly control your scapula during your rehabilitation exercises as well as during your everyday activities
Your physical therapist will also remind you about maintaining good shoulder posture even when sitting or using your upper limb during activities that are below shoulder height, such as working on the computer. Rounded shoulders in this position crowds the shoulder joint and can lead to shoulder impingement and pain. It should be noted that regaining proprioception of the shoulder girdle and upper limb requires concentrated work; most people have not previously needed to focus so intently on such controlled motion. The concentrated effort of these shoulder exercises, however, has a substantial reward as it plays a significant part in avoiding associated shoulder problems in the future once the original osteonecrosis problem has been dealt with.
It should be noted that physical therapy might be needed for extended periods of time. There are some patients whose osteonecrosis will continue to progress despite early conservative care. Unfortunately predicting who might develop a more advanced disease is difficult, so close monitoring is advised. If conservative care fails or the breakdown is too advanced to trial conservative care, surgery may be required.
STAR Physical Therapy provides services for physical therapy in Fairport and Rochester.
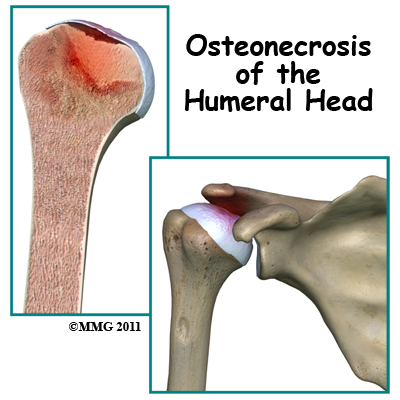 Osteonecrosis of the humeral head is a condition where a portion of the bone of the humeral head (the top of the humerus or upper arm bone) loses its blood supply, dies and collapses. Another term used for osteonecrosis is avascular necrosis. The term avascular means that a loss of blood supply to the area is the cause of the problem and necrosis means death.
Osteonecrosis of the humeral head is a condition where a portion of the bone of the humeral head (the top of the humerus or upper arm bone) loses its blood supply, dies and collapses. Another term used for osteonecrosis is avascular necrosis. The term avascular means that a loss of blood supply to the area is the cause of the problem and necrosis means death.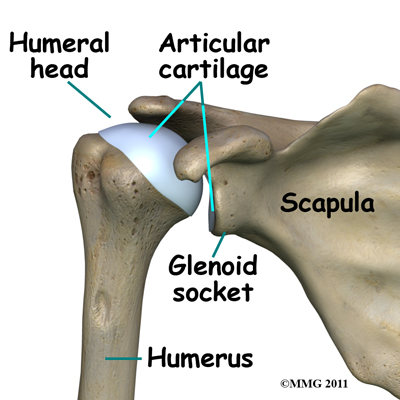
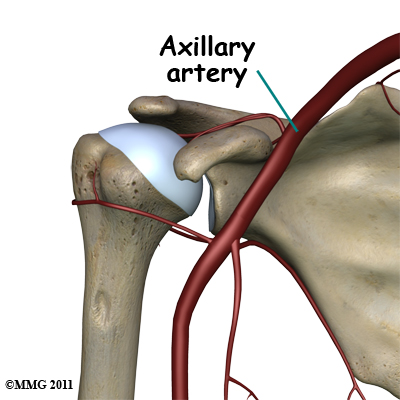
 Bone tissue is constantly being remodeled which means that old bone is removed and replaced with new bone. Osteonecrosis occurs when there is a loss of blood circulation in the bone of the humeral head. This causes the cells that remove and produce new bone to die in the area of lost circulation. New bone is no longer produced, but the old bone matrix still survives. Without the constant ability to repair itself through remodeling, the dead bone matrix eventually begins to lose strength and crumble. This causes the bone matrix to collapse. New blood vessels begin to grow into the area, but this is a slow process. The situation becomes a race to see whether new blood vessels will grow into the area and restore the ability to remodel the bone or whether bone collapse will occur.
Bone tissue is constantly being remodeled which means that old bone is removed and replaced with new bone. Osteonecrosis occurs when there is a loss of blood circulation in the bone of the humeral head. This causes the cells that remove and produce new bone to die in the area of lost circulation. New bone is no longer produced, but the old bone matrix still survives. Without the constant ability to repair itself through remodeling, the dead bone matrix eventually begins to lose strength and crumble. This causes the bone matrix to collapse. New blood vessels begin to grow into the area, but this is a slow process. The situation becomes a race to see whether new blood vessels will grow into the area and restore the ability to remodel the bone or whether bone collapse will occur.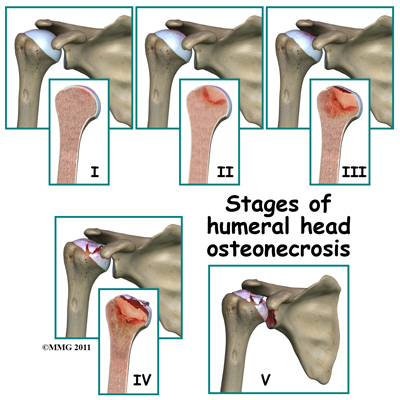
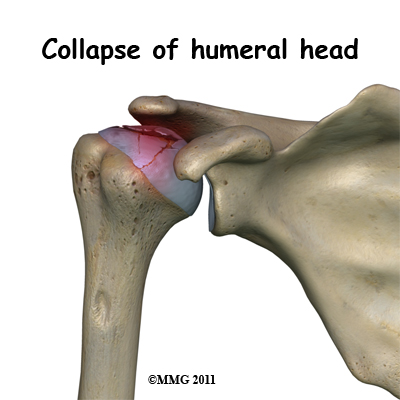
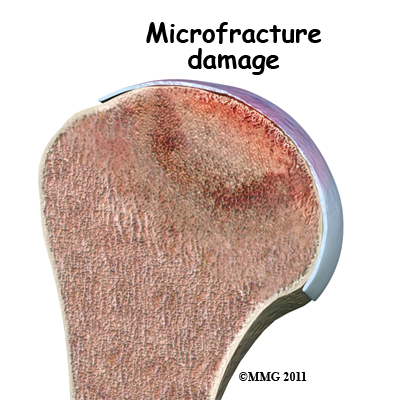 The first goal in treating osteonecrosis of the humeral head is to save the bone. Left untreated, the disease process will continue until the layer of bone just under the joint surface cracks causing small microfractures.
The first goal in treating osteonecrosis of the humeral head is to save the bone. Left untreated, the disease process will continue until the layer of bone just under the joint surface cracks causing small microfractures.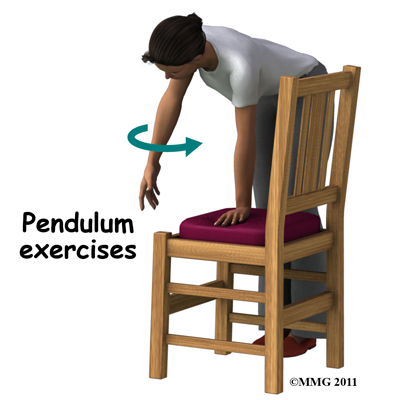 As soon as possible your therapist will begin to work on regaining your shoulder’s motion. They will teach you exercises that you can do yourself to assist with range of motion, which may include the use of sticks or pulleys to help raise the shoulder passively or your therapist may encourage you to partially use the muscles on your affected side (with the assistance of your good side) without causing discomfort. Doing pendular exercises can also help to maintain some shoulder range of motion and assist with pain at this stage. Pendular exercises are performed by leaning forward or to the side, letting the arm hang clear of the chest, and then initiating movement with your trunk so that the dangling limb passively and gently moves. This action provides some traction to the shoulder joint, which aids in pain relief, and also assists the shoulder into a relatively elevated position (in relation to the trunk.) It is important that the pendular activity is done as passively as possible without initiating motion
As soon as possible your therapist will begin to work on regaining your shoulder’s motion. They will teach you exercises that you can do yourself to assist with range of motion, which may include the use of sticks or pulleys to help raise the shoulder passively or your therapist may encourage you to partially use the muscles on your affected side (with the assistance of your good side) without causing discomfort. Doing pendular exercises can also help to maintain some shoulder range of motion and assist with pain at this stage. Pendular exercises are performed by leaning forward or to the side, letting the arm hang clear of the chest, and then initiating movement with your trunk so that the dangling limb passively and gently moves. This action provides some traction to the shoulder joint, which aids in pain relief, and also assists the shoulder into a relatively elevated position (in relation to the trunk.) It is important that the pendular activity is done as passively as possible without initiating motion 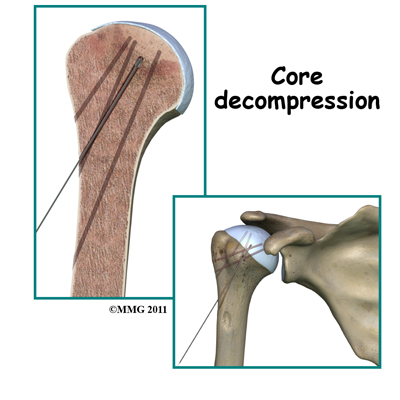 Surgical intervention may be needed in the more advanced stages of osteonecrosis. When the condition is in the early stages, a procedure called core decompression is used to reduce bone marrow pressure and allow the formation of a new blood supply to the area. The new blood vessels help the necrotic area start to form new, healthy bone.
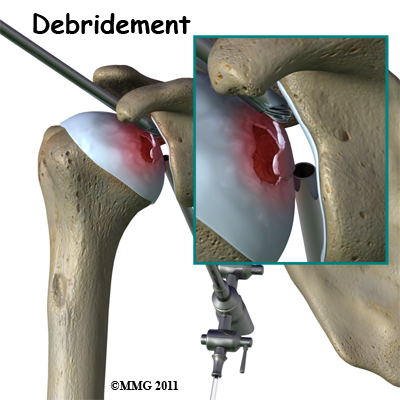
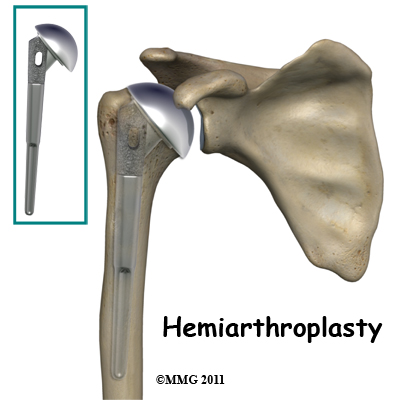
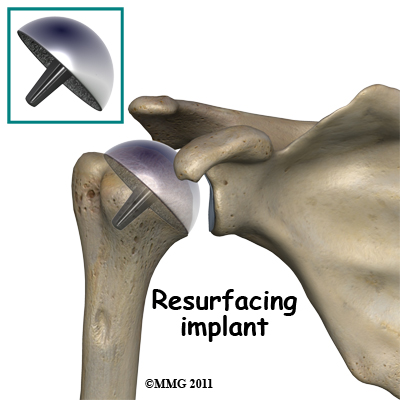
Surgical intervention may be needed in the more advanced stages of osteonecrosis. When the condition is in the early stages, a procedure called core decompression is used to reduce bone marrow pressure and allow the formation of a new blood supply to the area. The new blood vessels help the necrotic area start to form new, healthy bone.