What treatment options are available?
Non-surgical Treatment
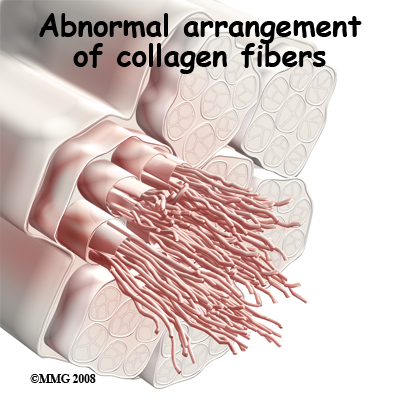
Patellar tendonitis is usually self-limiting. That means the condition will resolve with relative rest, activity modification, and physical therapy. Recurrence of the problem is common for patients who fail to let the patellar tendon recover fully before resuming training or other aggravating activities.
Although the time required for recovery varies, we typically recommend physical therapy for about four to six weeks. The aim of your STAR Physical Therapy treatment is to calm pain and inflammation, to correct muscle imbalances, and to improve the function of the quadriceps mechanism.
The initial treatment for acute patellar tendonitis begins by decreasing the inflammation in the knee. We may suggest relative rest and anti-inflammatory medications, such as aspirin or ibuprofen, especially when the problem is coming from overuse. Acetaminophen (Tylenol®) may be used for pain control if you can't take anti-inflammatory medications for any reason.
Relative rest is a term used to describe a process of rest-to-recovery based on the severity of symptoms. Pain at rest means strict rest and a short time of immobilization in a splint or brace is required. When pain is no longer present at rest, then a gradual increase in activity is allowed so long as the resting pain doesn't come back.
Physical therapy can help in the early stages by decreasing pain and inflammation. Your STAR Physical Therapy physical therapist may use ice massage, electrical stimulation, and ultrasound to limit pain and control (but not completely prevent) swelling. Some amount of inflammatory response is needed initially for a good healing response.
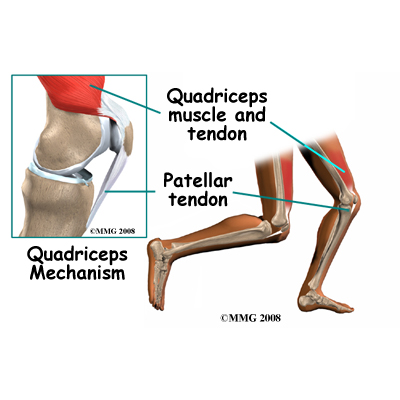
We will prescribe stretching and strengthening exercises to correct any muscle imbalances. Eccentric muscle strength training helps prevent and treat injuries that occur when high stresses are placed on the tendon during closed kinetic chain activities. Eccentric contractions occur as the contracted muscle lengthens. Closed kinetic chain activities means the foot is planted on the floor as the knee bends or straightens.
A specific protocol of exercises may be needed when rehabilitating this injury. After a five-minute warm up period, stretches are performed. Next, in a standing position, the patient bends the knees and drops quickly into a squatting position, and then stands up again quickly. The goal is to do this exercise as quickly as possible. Eventually sandbags are added to the shoulders to increase the load on the tendon. All exercises must be done without pain.
Researchers have also discovered that patellar tendonitis responds to a concentric-eccentric program of exercises for the anterior tibialis muscle. The anterior tibialis muscle is located along the front of the lower leg. It is the muscle that helps you dorsiflex the ankle (pull your toes and ankle up toward the knee).
You start with your foot in a position of full plantar flexion by rising up on your toes. Now drop down into a position of dorsiflexion. This is a concentric muscle contraction. Resistance of the foot and ankle from full dorsiflexion back into plantar flexion is the eccentric contraction. This exercise is repeated until the tibialis anterior fatigues. As your pain subsides, our program progresses so that eventually, you will just be doing the eccentric activities.
Flexibility exercises are often designed for the thigh and calf muscles. Specific exercises are used to maximize control and strength of the quadriceps muscles. We will show you how to ease back into jumping or running sports using good training techniques. Off-season strength training of the legs, particularly the quadriceps muscles is advised.
Bracing or taping the patella can help you do exercises and activities with less pain. Most braces for patellofemoral problems are made of soft fabric, such as cloth or neoprene. You slide them onto your knee like a sleeve. A small buttress pads the side of the patella to keep it lined up within the groove of the femur. An alternative to bracing is to tape the patella in place. Our physical therapist applies and adjusts the tape over the knee to help realign the patella. The idea is that by bracing or taping the knee, the patella stays in better alignment within the femoral groove. This in turn is thought to improve and retrain the pull of the quadriceps muscle so that the patella stays lined up in the groove, eventually without the brace. Patients report less pain and improved function with these forms of treatment.
If necessary, we may also design special shoe inserts called orthotics for you to improve knee alignment and function of the patella. Proper footwear for your sport is important, and we will advise you in this area.
Prevention of future injuries through patient education is a key component of our treatment program. This is true whether conservative care or surgical intervention is required. Modification of intrinsic and extrinsic risk factors is essential.
Coaches, trainers, and physical therapists can work together to design a training program that allows you to continue training without irritating the tendon and surrounding tissues. Remember to warm up and stretch before exercise. Some experts recommend a cool down and stretching after exercise as well. Know your limits and don't overdo it.
Use ice after activity if indicated by pain or swelling. Icing should be limited to no more than 15 minutes to avoid reflex vasodilation (increased circulation to the area to rewarm it causing further swelling). Heat may be used in cases of chronic tendonosis to stimulate blood circulation and promote tissue healing.
Whenever you have to miss exercising for any reason or when training for a specific event, adjust your training schedule accordingly. Avoid the "too" training errors mentioned earlier.
With our well-planned rehabilitation program, most patients are able to return to their previous level of activity without recurring symptoms.
Post-surgical Rehabilitation
Many surgeons will have their patients take part in formal physical therapy after knee surgery. More involved surgeries for patellar realignment or restorative procedures for tendon tissue require a delay before going to therapy. Rehabilitation may be slower to allow the tendon to heal before too much strain can be put on the knee.
When you begin your STAR Physical Therapy post-surgical rehabilitation program, the first few physical therapy treatments are designed to help control the pain and swelling from the surgery. Our therapist will choose exercises to help improve knee motion and to get the quadriceps muscles toned and active again. Muscle stimulation, using electrodes over the quadriceps muscle, may be needed at first to get the muscle moving again.
As the program evolves, we will choose more challenging exercises to safely advance your knee's strength and function. The key is to get the soft tissues in balance through safe stretching and gradual strengthening.
Our goal is to help you keep your pain under control, ensure you place only a safe amount of weight on the healing knee, and improve your strength and range of motion. When your recovery is well under way, regular visits to our office will end. Although we will continue to be a resource, you will be in charge of doing your exercises as part of an ongoing home program.
STAR Physical Therapy provides services for physical therapy in Fairport and Rochester.
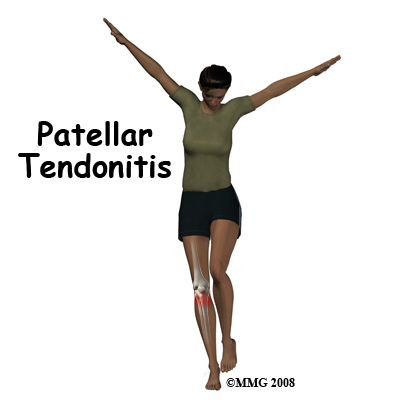
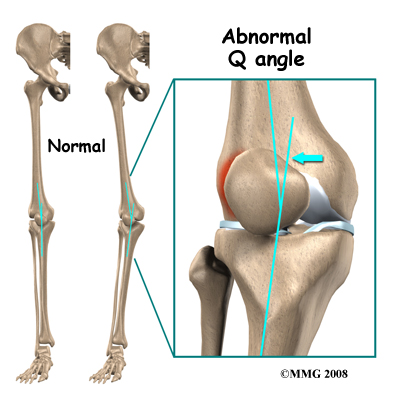
 Any muscle imbalance of the lower extremity from the hip down to the toes can impact the quadriceps muscle and affect the joint. Individuals who are overweight may have added issues with load and muscle imbalance leading to patellar tendonitis.
Any muscle imbalance of the lower extremity from the hip down to the toes can impact the quadriceps muscle and affect the joint. Individuals who are overweight may have added issues with load and muscle imbalance leading to patellar tendonitis.