No hard and fast rule exists as to when surgery is needed. Surgery is usually recommended when the joint at the knuckle of the finger reaches 30 degrees of flexion. When patients have severe problems and require surgery at a younger age, the problem often comes back later in life. When the problem comes back or causes severe contractures, surgeons may decide to fuse the individual finger joints together. In the worst case, amputation of the finger may be needed if the contracture restricts the nerves or blood supply to the finger.
Surgery for the main knuckle of the finger (at the base of the finger) has better long-term results than when the joint in the middle of the finger is affected. A contracture is more likely to return after surgery for the middle joint.
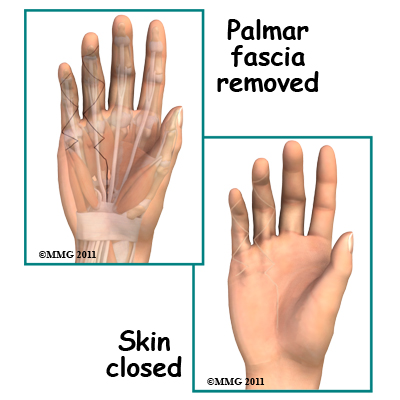
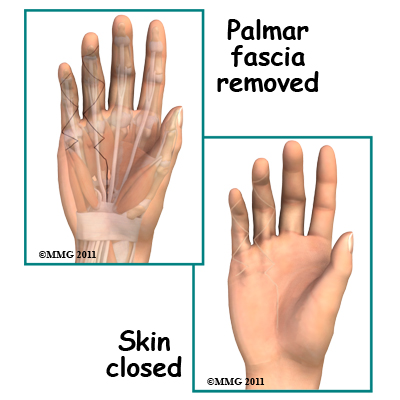
The goal of tissue release surgery is to release the fibrous attachments between the palmar fascia and the tissues around it, thereby releasing the contracture. Once released, finger movement should be restored to normal. If the problem is not severe, it may be possible to free the contracture simply by cutting the cord under the skin. If the palmar fascia is more involved and more than one finger is bent, your surgeon may take out a large portion of the sheet of fascia.
This remains the gold standard of treatment for Dupuytren's contracture. Removal of the diseased palmar fascia will usually give a very good result. The cure is often permanent but depends a great deal on the success of doing the physical therapy post surgically as prescribed. Removing the palmar fascia causes little ill effect, although the fingers may bend backward slightly more than normal. If you decide to have this surgery, it is pertinent that you commit to doing the therapy needed to make your surgery as successful as possible.
Removal of the entire palmar fascia (radical fasciectomy) requires extensive removal of involved and non-involved palmar and digital (finger) fascia. This approach may be required but it has higher complications rates without providing better success rates so it is no longer done commonly.
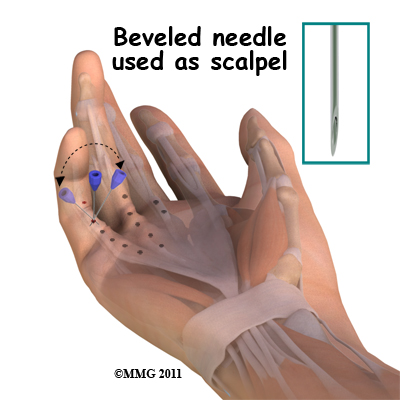
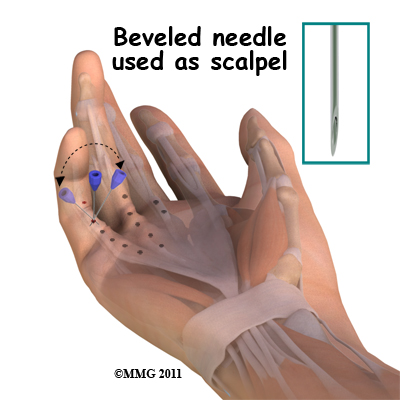
A less invasive procedure called a needle aponeurotomy (also referred to as a percutaneous fasciotomy) is available when the disease is at an early stage. Under local anesthesia, the surgeon inserts a very thin needle under the skin. The sharp needle cuts a path through the cord, weakening it enough to stretch and extend it, or rupture it.
The advantage of this procedure is that it can be done on older adults who have other health issues that might make surgery under general anesthesia too risky. The disadvantage is a high recurrence rate and the potential for nerve injury, infection, and hematoma (pocket of blood) formation.This procedure, however, has replaced the fasciectomy in many practices.
A skin graft may be needed if the skin surface has contracted so much that the fingercannot relax as it should and the palm cannot be stretched out flat. Surgeons graft skin from the wrist, elbow, or groin. The skin is grafted into the area near the incision to give the finger extra mobility for movement.
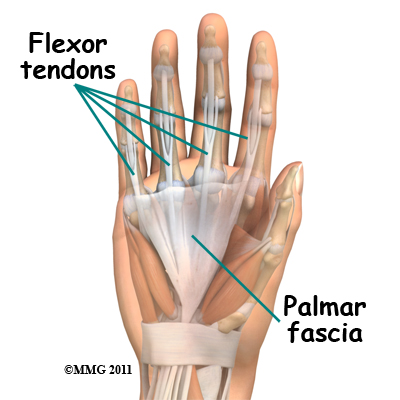 Blood vessels carry needed oxygen, nutrients, and fuel to the muscles to allow them to work normally and heal when injured. Tendons and ligaments are connective tissue. Another type of connective tissue, called fascia, surrounds and separates the tendons and muscles of the hand.
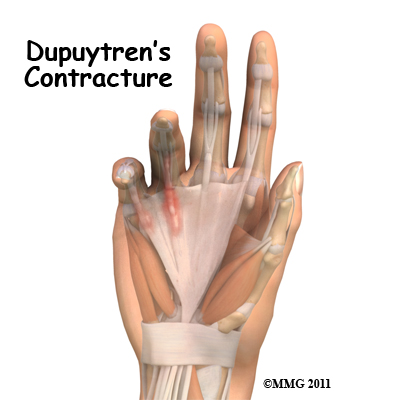
Blood vessels carry needed oxygen, nutrients, and fuel to the muscles to allow them to work normally and heal when injured. Tendons and ligaments are connective tissue. Another type of connective tissue, called fascia, surrounds and separates the tendons and muscles of the hand. Normally, we are able to control when we bend our fingers and how much. How much we flex our fingers determines how small an object we can hold and how tightly we can hold it. This control is lost as the disorder develops and the palmar fascia contracts, or tightens. The contracture is like extra scar tissue just under the skin. As the disorder progresses, the bending of the finger becomes more and more severe, which limits the motion of the finger.
Normally, we are able to control when we bend our fingers and how much. How much we flex our fingers determines how small an object we can hold and how tightly we can hold it. This control is lost as the disorder develops and the palmar fascia contracts, or tightens. The contracture is like extra scar tissue just under the skin. As the disorder progresses, the bending of the finger becomes more and more severe, which limits the motion of the finger.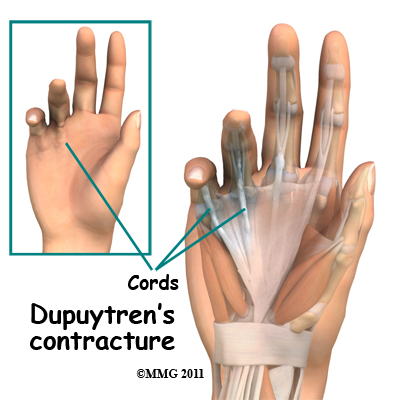
 Ongoing research of this condition has resulted in a less invasive nonsurgical method of treatment called an enzymatic fasciotomy. If it is the main knuckle of the finger (at the base of the finger) that is contracted, and there are only one or two cords involved, this procedure may be possible. For this treatment, a new injectable drug, Xiaflex, which is gaining popularity and approval for use around the world, is used. By injecting an enzyme directly into the cords formed by the disease, the tissue dissolves and starts to weaken, most often the patients are able to break apart the cord by themselves.
Ongoing research of this condition has resulted in a less invasive nonsurgical method of treatment called an enzymatic fasciotomy. If it is the main knuckle of the finger (at the base of the finger) that is contracted, and there are only one or two cords involved, this procedure may be possible. For this treatment, a new injectable drug, Xiaflex, which is gaining popularity and approval for use around the world, is used. By injecting an enzyme directly into the cords formed by the disease, the tissue dissolves and starts to weaken, most often the patients are able to break apart the cord by themselves.