Non-surgical Rehabilitation
Treatment usually begins when the joint first becomes painful. This may only occur with heavy use and may simply require mild anti-inflammatory medications, such as aspirin or ibuprofen. Reducing the activity, or changing from occupations that require heavy repetitive hand and finger motions, may be necessary to help control the symptoms.
Our primary goal is to help you learn how to control symptoms and maximize the health of your hand and fingers. When you visit STAR Physical Therapy in Fairport and Rochester, our physical therapist will instruct you in ways to calm pain and symptoms, which might include the use of rest, heat, or topical rubs.
We will then begin range-of-motion exercises for your finger after your pain eases, followed by a program of strengthening to improve your finger movement. Strengthening exercises for the arm and hand help steady the hand and protect the finger joints from shock and stress. Our therapist may also use dexterity and fine motor exercises to get your hand and fingers moving. We will go over tips on how you can get your tasks done with less strain on the joint.
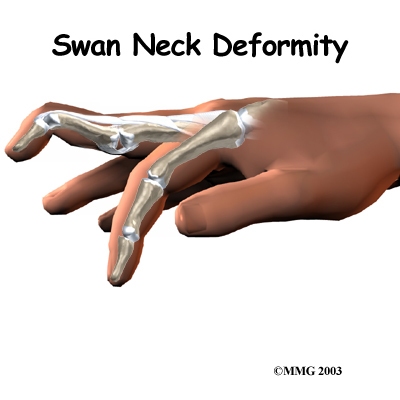
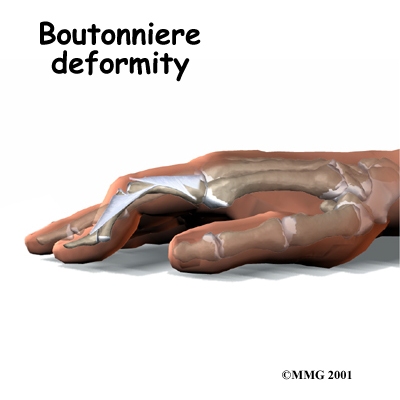
Your physical therapist may recommend a custom finger brace or splint to support your finger joints. These devices are designed to help reduce pain, prevent deformity, or keep a finger deformity from getting worse.
Post-surgical Rehabilitation
Your hand will be bandaged with a well-padded dressing and a finger splint for support after surgery. Although time required for recovery varies among patients, you may need to attend our physical or occupational therapy sessions after surgery for up to eight weeks.
When you begin your STAR Physical Therapy post-surgical physical therapy program, the first few treatments will be used to help control the pain and swelling after surgery. Some of the exercises that our physical therapist will have you do help strengthen and stabilize the muscles around the finger joint. We’ll recommend other exercises to improve the fine motor control and dexterity of your hand. Our physical therapist will also give you tips on ways to do your activities while avoiding extra strain on the finger joint.
At STAR Physical Therapy, our goal is to help you keep your pain under control, improve your range of motion, and maximize strength and control in your finger. When your recovery is well under way, regular visits to our office will end. Our physical therapist will give you tips on keeping your symptoms controlled. We will continue to be a resource, but you will be in charge of doing your exercises as part of an ongoing home program.
STAR Physical Therapy provides services for physical therapy in Fairport and Rochester.

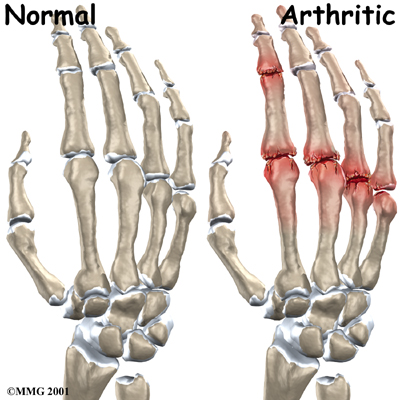
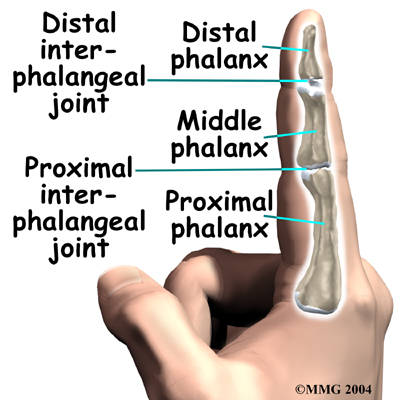 The bones in the palm of the hand are called metacarpals. One metacarpal connects to each finger and thumb. Small bone shafts called phalanges line up to form each finger and thumb.
The bones in the palm of the hand are called metacarpals. One metacarpal connects to each finger and thumb. Small bone shafts called phalanges line up to form each finger and thumb. Related Document:
Related Document: