What parts of the foot are involved?
The anatomy of the foot is very complex. When everything works together, the foot functions correctly. When one part becomes damaged, it can affect every other part of the foot and lead to problems. With a flatfoot deformity, bones, ligaments, and muscles of the foot are all affected. Areas up the biomechanical chain such as the ankle, the shin, the knee, the hip and the low back can also be affected due to the misalignment that occurs.
Related Document: STAR Physical Therapy's Guide to Foot Anatomy
Bones
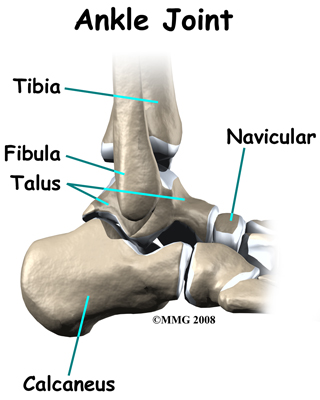
The skeleton of the foot centers around the talus, or ankle bone, that forms the main part of the ankle joint. The two bones of the lower leg, the large tibia and the smaller fibula, come together at the ankle joint around the talus to form a very stable structure.
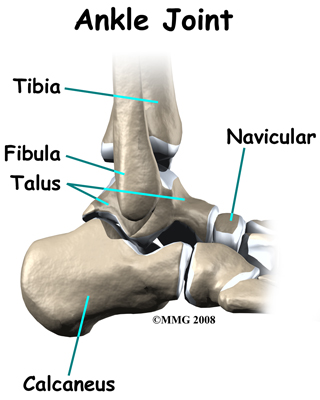 The foot is able to bend up and down due to the joint formed by the tibia, fibula, and talus.
The foot is able to bend up and down due to the joint formed by the tibia, fibula, and talus.
The two bones that make up the back part of the foot (sometimes referred to as the hindfoot) are the talus and the calcaneus. The calcaneus is the heel bone. The talus is connected to the calcaneus at the subtalar joint. The subtalar joint allows the foot to rock from side to side. People with flatfeet usually have more motion at the subtalar joint than people who do not have flatfeet. This increased flexibility of the subtalar joint results in many compensatory actions of the foot and ankle in order to maintain proper foot alignment during standing and walking.
Just down the foot from the ankle is a set of five bones called tarsal bones that work together as a group and are termed the midfoot. These tarsal bones are unique in the way they fit together. There are multiple joints between the tarsal bones. When the muscles of the foot and leg twist the foot inwards, these bones lock together and form a very rigid structure. When they are twisted in the opposite direction, they become unlocked and allow the foot to conform to whatever surface the foot is contacting.
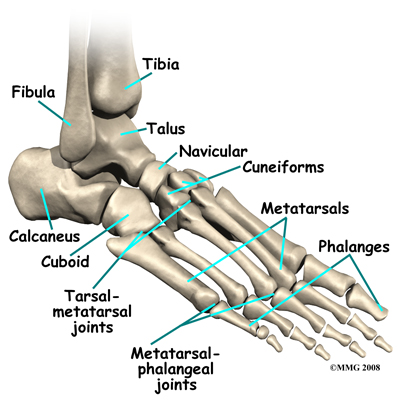
The tarsal bones are connected to the five long bones of the foot called the metatarsals. The two groups of bones are fairly rigidly connected, without much movement at the joints that connect them. Finally, there are the bones of the toes, called the phalanges. The metatarsals and phalanges make up the forefoot.
Ligaments and Tendons
Ligaments are the soft tissues that attach bones to bones. Ligaments are very similar to tendons in their make up however tendons attach muscles to bones rather than bones to other bones. Both of these structures are made up of small fibers of a material called collagen. The collagen fibers are bundled together to form a rope-like structure.
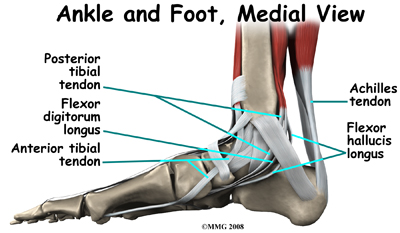
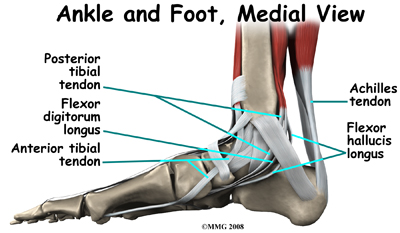
The large Achilles' tendon, at the back of the ankle is the most important tendon for walking, running, and jumping. It attaches the calf muscles to the heel bone to allow us to rise up on our toes. The posterior tibial tendon attaches one of the smaller muscles of the calf to the underside of the foot. This tendon helps support the arch and allows us to turn the foot inward. Failure of the posterior tibial tendon is a major problem in many cases of pes planus.
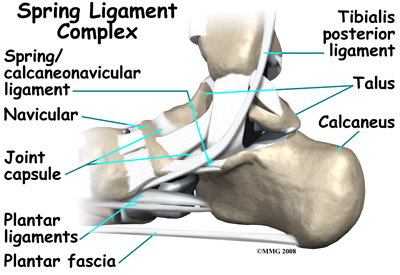
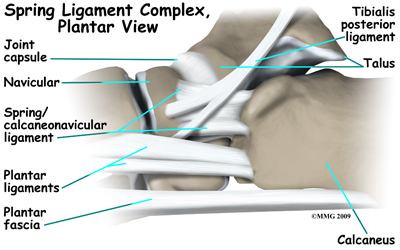
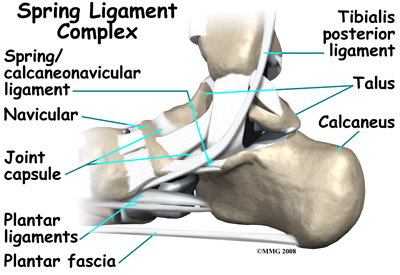
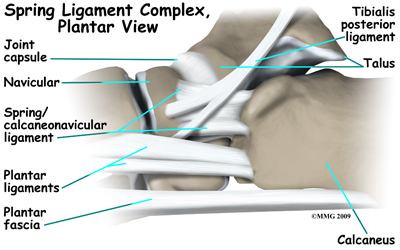
Many small ligaments hold the bones of the foot together. Most of these ligaments form part of the joint capsule around each of the joints of the foot. A joint capsule is a watertight sac that forms around all of the joints of the foot. The capsule is made up of the ligaments around the joint and the soft tissues between the ligaments that fill in the gaps and form the sac.
The plantar fascia is a thick band of ligamentous tissue on the bottom of the foot that extends from the heel to the toes. When you pull your toes back with one hand, you will be able to feel this band with your fingers of the other hand. This fascia is also critical in supporting the long arch of the foot and in creating the rigid foot structure mentioned above.
The spring ligament complex, which supports the talonavicular joint, is often involved in the flatfoot condition. The spring ligament complex works with the posterior tibial tendon and the plantar fascia to support and stabilize the longitudinal arch of the foot. Laxity of the ligaments that support this arch can result in deformity of the foot and/or ankle resulting in pes planus.
Foot Anatomy Ligaments & Tendons
Muscles
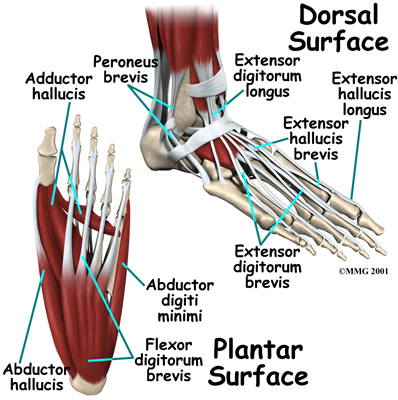 The strong muscles and tendons in the lower leg that connect directly to the foot create most of the motion of the foot. Contraction of these muscles is the main way that we move our feet to stand, walk, run, and jump.
The strong muscles and tendons in the lower leg that connect directly to the foot create most of the motion of the foot. Contraction of these muscles is the main way that we move our feet to stand, walk, run, and jump.
There are numerous small muscles in the foot. While these muscles are not nearly as important as the similar small muscles in the hand, they do affect the way that the toes work. Most of the muscles of the foot are arranged in layers on the sole of the foot (the plantar surface). There they connect to and move the toes as well as provide padding underneath the sole of the foot. Damage to these muscles can cause problems in the foot.
 The foot is able to bend up and down due to the joint formed by the tibia, fibula, and talus.
The foot is able to bend up and down due to the joint formed by the tibia, fibula, and talus.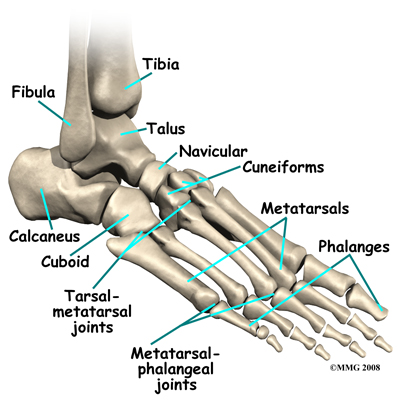
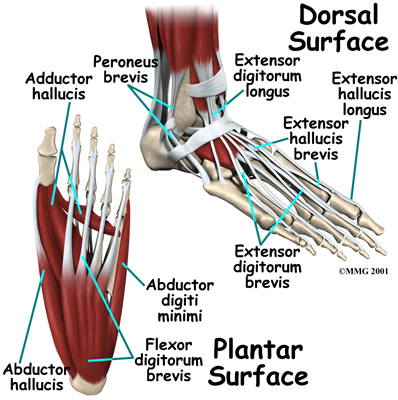 The strong muscles and tendons in the lower leg that connect directly to the foot create most of the motion of the foot. Contraction of these muscles is the main way that we move our feet to stand, walk, run, and jump.
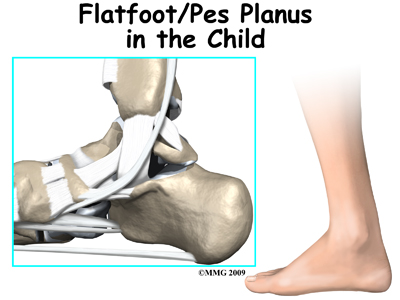
The strong muscles and tendons in the lower leg that connect directly to the foot create most of the motion of the foot. Contraction of these muscles is the main way that we move our feet to stand, walk, run, and jump.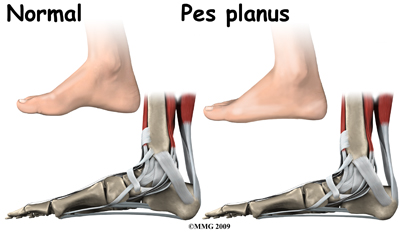 Most babies and young children have what looks like flat feet but this is normal for them. In a baby much of the foot and ankle are still made up of soft tissue, fat, and cartilage and the arch has not formed fully yet. Eventually as the baby gets older the cartilage calcifies into the normal bones of the foot. When the child starts to get up on their feet to begin walking the joints are still hypermobile. This is when the flatfoot deformity becomes obvious and parents may become concerned that something is wrong with their child's foot. The vast majority of children will grow out of the flat foot within their first decade of life. Stress and activities during early childhood requiring strength in the feet are actually the training needed to develop normal muscle, tendon, ligaments, and bone in the foot and ankle. In some cases, unfortunately, the arch doesn't form and the foot remains flat into late childhood, adolescence, and adulthood.
Most babies and young children have what looks like flat feet but this is normal for them. In a baby much of the foot and ankle are still made up of soft tissue, fat, and cartilage and the arch has not formed fully yet. Eventually as the baby gets older the cartilage calcifies into the normal bones of the foot. When the child starts to get up on their feet to begin walking the joints are still hypermobile. This is when the flatfoot deformity becomes obvious and parents may become concerned that something is wrong with their child's foot. The vast majority of children will grow out of the flat foot within their first decade of life. Stress and activities during early childhood requiring strength in the feet are actually the training needed to develop normal muscle, tendon, ligaments, and bone in the foot and ankle. In some cases, unfortunately, the arch doesn't form and the foot remains flat into late childhood, adolescence, and adulthood.