What happens during elbow fusion surgery?
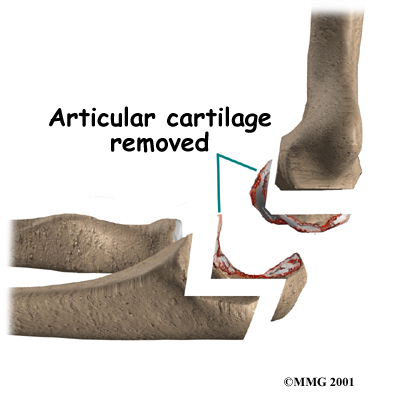
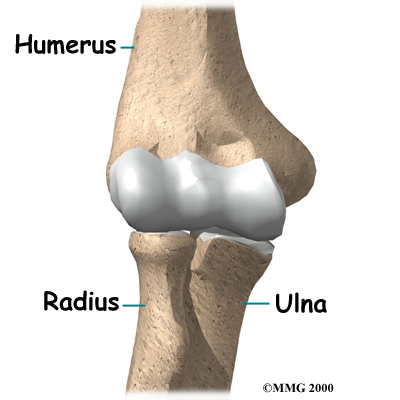
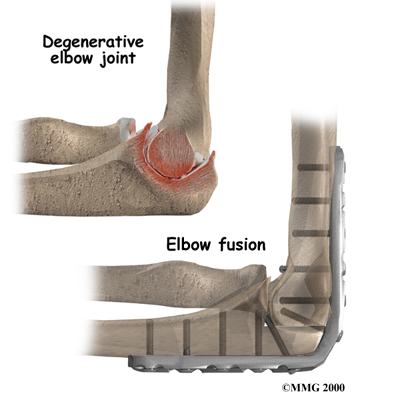
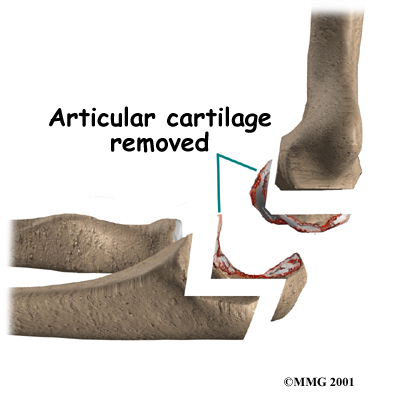
There are many different types of operations to fuse the elbow. Most of the procedures are designed to remove the articular cartilage from the joint surfaces of the hinge joint and then bind the two surfaces together until they heal. When two raw bone surfaces are held together like this, your body treats them like a broken bone. New bone forms to heal the two pieces together. When the fusion is healed, a strong, solid connection between the humerus and ulna will have replaced the painful arthritic joint.
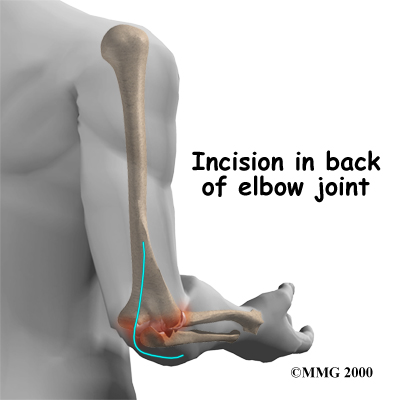
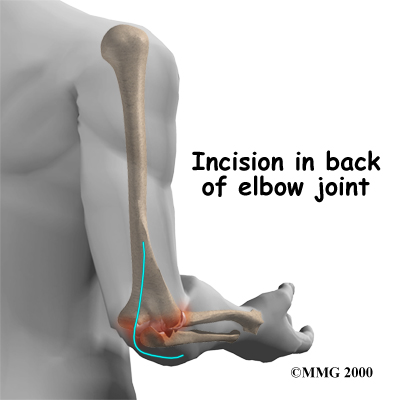
The first step in an elbow fusion is an down the back of the elbow. The incision is made on the back side because most of the blood vessels and nerves are on the inside of the elbow. Entering through the back of the elbow makes them less likely to be damaged.
The surgeon then moves the tendons and ligaments to the side to expose the joint surfaces. Care must be taken to protect the nerves that run beside the elbow joint on their way to the hand. The surgeon then surface of each side of the joint.
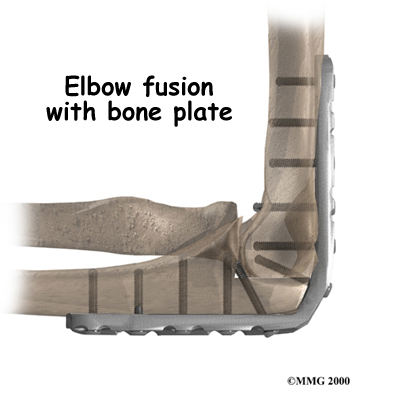
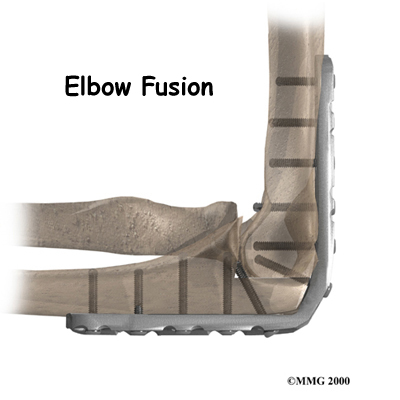
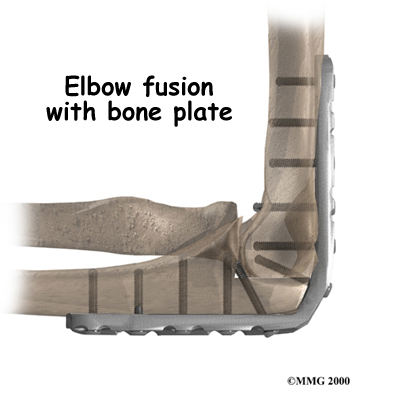
The surgeon must then fix the humerus and ulna in place until they can heal together. The elbow is bent to 90 degrees and the bones are carefully aligned. The bones must be properly aligned and immobilized for fusion to occur.
Plate Fixation
There are different ways of holding the bones together. Many surgeons place a with screw holes onto the back of the elbow, from the humerus to the ulna. The metal plate is attached to the bone with metal screws. The metal plate stays in the arm permanently. It is only removed if it causes problems.
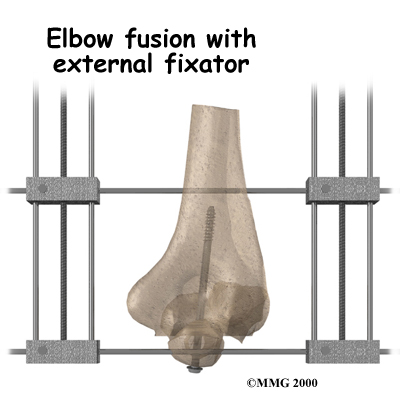
External Fixation
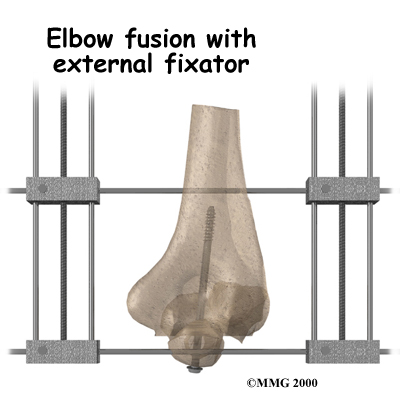 Another way to hold the bones together is to use an . Surgeons sometimes choose an external fixator if there have been problems with an infection in the elbow joint.
Another way to hold the bones together is to use an . Surgeons sometimes choose an external fixator if there have been problems with an infection in the elbow joint.
An external fixator involves placing metal pins through the bones above and below the elbow joint. Your surgeon may also place a metal screw inside the ulna and humerus to pull the bones together. The external fixator device is then placed on the elbow outside the skin, after the incision is sewn up. The external fixator attaches to the metal pins, which come through the skin, with metal rods and bolts.
At the end of the fusion operation, the incisions are sutured together. As long as you don't have an external fixator, the arm is placed in a large splint or cast. It usually takes about 12 weeks for the fusion to become solid. At this point the metal pins and rods of the external fixator are removed.
Patients who have an external fixator should expect to wear it for up to 12 weeks. When a cast is used, some doctors will replace it with a removable splint after six to eight weeks. If you wear a cast, the joints in your wrist and fingers may feel stiff or sore.
Your surgeon will X-ray your elbow several times after surgery to make sure that the bones are healing properly. Once your surgeon is sure that fusion has occurred, you can safely begin a strengthening program. It will take some time to regain the strength in your arm. As with any surgery, you need to avoid doing too much, too quickly.
 Another way to hold the bones together is to use an
Another way to hold the bones together is to use an