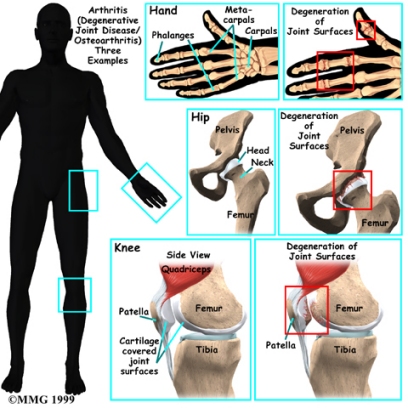
Where does OA develop?
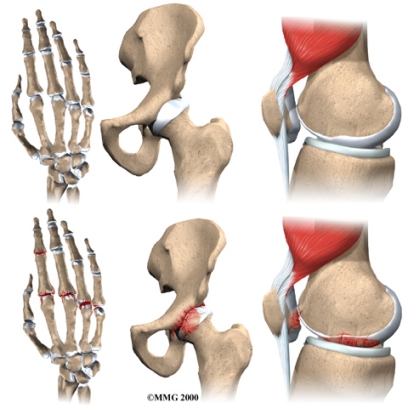
OA is most common in the small joints of the hands, the spine, the knees, the hips, and certain toe joints. OA primarily affects the articular cartilage, the slippery, cushioned surface that covers the ends of the bones in most joints and lets the bones slide without rubbing. Articular cartilage also functions as a shock absorber.
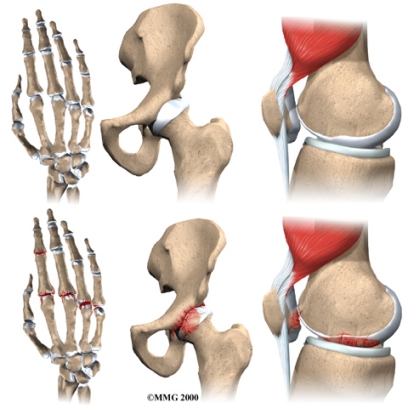
In OA, the articular cartilage becomes damaged or worn away. As this happens, the joint no longer fits together well or moves smoothly. In the early stages of OA, the cartilage actually becomes thicker as your body tries to repair the damage. The repaired areas are more brittle than the original cartilage, and these brittle areas begin to wear away and become thin. They may even wear away entirely. This eventually leads to a condition called eburnation, in which the bones become thick and polished as they rub together. X-rays can show these changes in the cartilage and bones.
But OA is not just a disease of the cartilage. The damage to the cartilage seems to start a sort of chain reaction that involves all the parts of the joint. Bone spurs, or outgrowths, often begin to form around the edges of the joint. The joint capsule (the watertight sack around the joint) can become thickened and lose its stretch. The synovial membrane that lines the inside of the joint capsule may become inflamed (swollen, red, hot, and painful), and crystals may form in the synovial fluid. The tendons and ligaments around the joint can also become inflamed.
Even the muscles around the joint can lose their strength. This usually occurs as a result of under-use of the muscles due to pain in the joint. When something hurts we subconsciously change the way we use the joint to avoid the pain. This causes the muscles to become weakened. Cartilage itself does not have nerves to feel pain, therefore the pain of OA probably comes from these other changes in and around the joint.